The cervix is the bottom of the uterus. In the upper part of the uterus (body), the fruit is born and developed. The cervix connects the body of the uterus with the vagina (generic channel). Cervical cancer develops from the epithelium that lins the cervix. Normal cervical cells are first subjected to changes and become prepubrase, and then turn into cancer.
Content
Two main types of cervical cancer are distinguished: flat-chip cancer and adenocarcinoma. Diagnosis of cervical cancer and prematubological states is determined as a result of microscopic research.
In 80-90% of cases, cervical tumors are represented by flat-belling cancer. The remaining 10-20% constitute adenocarcinoma. Adenokarcinoma are more common in women born in the last 20-30 years. Sometimes the cervical cancer has a feature of both flat-stacked cancer and adenocarcinoma (mixed carcinomas).
Some women with preoperative changes of the cervix arises cancer. This process usually takes several years, but sometimes flows within one year. Most women have preoperative cells disappear without treatment.
However, if these preproxy states are treated, then almost all the true forms of cervical cancer can be prevented.
Cancer cervical cancer
In recent years, some risk factors have been identified that increase the likelihood of cervical cancer.
Human papilloma virus (HPV). The infection caused by the human papilloma virus (HPV) is transmitted from person to person sexually and is the most important risk factor in the development of cervical cancer.

Normal cells produce substances (genes depressing tumor growth), which prevent too fast cell growth and turn them into tumor. Two proteins (E6 and E7), which are produced by some types of human papillomas virus, can change the function of gene substances that depress tumor growth.
However, HPV infection does not fully explain the reason for the development of cervical cancer, since neither all women with such an infection arises cervical cancer.
Smoking. During smoking, carcinogenic substances appear, damaging the DNA of the cervical cells, which can contribute to the development of cancer.
Deficiency of the immune system. The immune system protects us from cancer. AIDS virus makes the immune system of a woman less able to resist human papilloma virus and early cervical cancer.
Poor food Low consumption of fruits and vegetables also increases the risk of cervical cancer.
What are the risk factors cervical cancer?
Risk factor is all that increases the likelihood of cancer. However, the presence of one or even several risk factors still does not mean the likelihood of disease.
Some factors increase the risk of cervical cancer. In women who have no risk factors, cancer is rare. However, many women with risk factors, cervical cancer may not arise at all.
When a woman is diagnosed with a cervical cancer or a prematurity state, it is often difficult to determine which risk factors was the cause of the disease.
Knowledge of risk factors need for many reasons. First, some of them can be changed, for example, smoking and sex contacts, which can lead to infection with the human papilloma virus (HPV).
Some risk factors cannot be changed, including age or family history. Secondly, knowledge of risk factors can contribute to the survey with the purpose of early diagnosis of cervical cancer (the study of the swabs of the cervix).
Recommendations for early detection of cervical cancer
- All women should undergo screening (twisted examination) on cervical cancer 3 years after the start of sexual life, but not later than 21 years. Screening must be carried out annually with the study of swabs from the cervix.
- Starting from 30 years of age, women who had three consecutive negative results in the study of cervical marshs can be screened every 2-3 years. Women with Calovek's papilloma virus or a weakened immune system as a result of transplantation, chemotherapy or long-term use of steroid hormones, should continue annual screening.
- Women are 70 years and older with three and more normal results of the study of the cervical marsh over the past 10 years may not participate in screening. Women who suffered cervical cancer, having HPV or a weakened immune system, should continue screening while they allow them to health.
- Women who suffered the removal of the uterus and cervix may not participate in screening if the operation was performed not about cancer or the precancerous state of the cervix. Women who produced the removal of the uterus without removing the cervix must continue to participate in screening.

Some women believe that they should not be examined due to the fact that they are no longer going to have children. Such a point vision is incorrect.
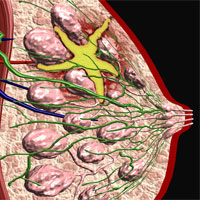
Study of the pelvis organs is part of a woman survey. In this study, the doctor assesses the state of reproductive bodies, including the uterus and ovaries, and can also identify sexually transmitted diseases. However, with this study, it is impossible to diagnose cervical cancer at an early stage or detect the modified cervical cells.
Mashers from the cervix are performed before the start of the inspection of the pelvis organs, while the doctor with the help of a special tool receives a certain number of cells from the cervix, which are then investigated under the microscope.
Other malignant tumors: Melanoma, sarcoma and lymphoma can also occur in the cervix, but these tumors are very rare.
Colposcopy: If, according to the examination of the examination, cervical cancer is suspected, then the execution of colposcopy is recommended. With this procedure, the doctor examines the neck of the uterus by the colposcope (apparatus with increasing lenses). In this case, the surface of the cervix is investigated in detail. When a suspicious area is found, biopsy (taking a small piece of fabric for research). Only biopsy allows you to judge with confidence about whether a woman has a prematurity state, a true cancer or something else.
In case of identifying suspicious changes in cervical cells, cryosurgery can be offered (using liquid nitrogen) or laser surgery.
These two methods almost always allow to cure a prepubilate disease and prevent cancer.
Treatment of cervical cancer
Stage (prevalence) of the process is the main thing in solving the issue of the treatment of cervical cancer. However, when choosing a method of therapy, the location of the tumor on the cervix, the tumor type (flat-mellular cancer or adenocarcinoma), your age, the general condition and desire to have children.
With the earliest stage of the cervical cervix (carcinoma), cryosurgery, laser surgery, excision of the tumor of electrical loop and conizenction (wedge-shaped removal of the cervical cervix). In the case of a relapse (return) of the tumor or reluctance to have in the future children can be offered simple hysterectomy (uterus removal).
In patients with more common stages of cervical cancer, usually perform advanced hysterectomy (removal of the uterus together with lymph nodes) in combination with one type of radiation therapy and sometimes chemotherapy.
The survival of patients with 0, I and II stages of the disease ranges from 65 to 95% and the better the lower the cancer stage.
In women with the III-IV stages of cervical cancer, internal and external irradiation are used, as well as chemotherapy. In this case, the survival rate of this category of patients varies from 20 to 50%.
In case of recurrence of cervical cancer, treatment depends on the type of recurrence. Under local recurrence, extended operations may be effective in 40-50% of women. In women with remote metastases (in the liver or bones), chemotherapy may lead to a temporary improvement in 15-25% of cases.