Sphinction dysfunction Oddi develops after removal of the gallbladder hardly in every third case. The post-olecistectomic syndrome and the treatment of this state will go a conversation in our article.
Content
- How to prevent the development of postcholecystectomic syndrome?
- What to do if there are signs of PSES?
- Postcholecistectomic syndrome: Treatment
- In second place in importance, medical therapy is worth.
- When the re-operation is shown?
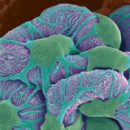
 Oddi's sphincter dysfunction or postcholectomic syndrome (PCP) develops after removing the gallbladder hardly in each third case. And the case is not at all in the defects of the operation, but in the fact that in itself it does not eliminate the causes of the development of gallstone disease. Bile — still retains the lithogenic properties and the formation of stones in the ducts can not be excluded. Moreover, the removal of the gallbladder becomes the cause of the dysfunction of the locking sphincter Oddi, regulating the receipt of the bile and pancreatic juices in the intestine and causes digestive disorders.
Oddi's sphincter dysfunction or postcholectomic syndrome (PCP) develops after removing the gallbladder hardly in each third case. And the case is not at all in the defects of the operation, but in the fact that in itself it does not eliminate the causes of the development of gallstone disease. Bile — still retains the lithogenic properties and the formation of stones in the ducts can not be excluded. Moreover, the removal of the gallbladder becomes the cause of the dysfunction of the locking sphincter Oddi, regulating the receipt of the bile and pancreatic juices in the intestine and causes digestive disorders.
How to prevent the development of postcholecystectomic syndrome?
Specific prevention of postcholectectomic syndrome does not exist. Of course, the probability of developing this state increases if the operation is performed by a low qualification surgeon, however, the timeliness of intervention and quality of postoperative rehabilitation plays a major role. The only possible way to prevent PHES can be considered cholecystectomy in a quiet period, that is, outside the attack of cholecystitis, and compliance with all the recommendations of the doctor after removing the bubble.
What to do if there are signs of PSES?
If after the operation still worries discomfort in the abdomen, if pain attacks occur periodically, accompanied by nausea and vomiting, if the diagrams alternate with constipation, and the meteorism delivers inconvenience, you should seek help. Only close interaction with the doctor will make it possible to find the causes of postcholycystectomic syndrome and choose a treatment that will save from his symptoms.
When signs of postoperative sphincter dysfunction are best to turn to a specialist who conducted cholecystectomy. In the absence of such a possibility, treatment can be held in any multidisciplinary medical institution with the branch of Abdominal Surgery.
Postcholecistectomic syndrome: Treatment
Since the symptoms of post-olecistectomic syndrome are primarily associated with a violation of the current of the bile and pancreatic secret, the treatment is aimed at eliminating obstacles and normalization of the receipt of these juices in the duodenum.
Treatment of postcholectectomic syndrome includes:
- correction of the composition and rheological properties of bile;
- Normalization of the Sphinteer's Pateuries;
- normalization of the bowelosis of the intestine;
- normalization of motility of the small intestine;
- Optimization of digestion processes.
Perhaps the main place in the treatment of PCPs occupies dietherapy. Power is adjusted in accordance with the deadlines for postcholycystectomic syndrome and its type, with the initial mass of the body of the patient and the composition of the bile.
In second place in importance, medical therapy is worth.
 Antispasmodic drugs are prescribed to eliminate sphincter Sphinte. For this purpose, nitrates, anticholinergic agents, non-selective and selective m-cholinoblocators, block plates of slow calcium channels, myotropic spasmolytics. A good effect gives a dressing, having a selective action on the muscles of the sphincter Oddi.
Antispasmodic drugs are prescribed to eliminate sphincter Sphinte. For this purpose, nitrates, anticholinergic agents, non-selective and selective m-cholinoblocators, block plates of slow calcium channels, myotropic spasmolytics. A good effect gives a dressing, having a selective action on the muscles of the sphincter Oddi.- Antibacterial therapy is mandatory with such a disease as postcholycistectomic syndrome, treatment includes 1-2 courses of antibiotics and aimed at the destruction of pathological microflora, which causes the processes of fermentation and rotting in the intestine. After the course of antibiotic therapy, prebiotics and probiotics are prescribed, contributing to the restoration of normal intestinal biocenosis, the normalization of digestion.
- To eliminate constipation showing laxatives, for example, Duhalak.
- To eliminate dyspepsia, in particular heartburn, aluminum containing antacids are prescribed.
- In pronounced disorders of digestion and enzymatic failure, enzyme preparations are shown.
- To reduce the ability of bile to stone formation, uroz and hanodoxicole acid preparations are used.
- To maintain and restore liver, drugs such as heptral, LIV52, Essentialy.
When the re-operation is shown?
Absolute testimony to surgery are:
- Stenosis or scar suspension of the Sphinteer Appa;
- recurrent (repeated) pancreatitis;
- Lack of effect from medication treatment of PSES.
What operations are conducted? It all depends on the specific case, but most often resort to endoscopic sphincteroplastic, which implies the dissection of the muscle compound between the pancreatic duct and the common bile duct.