Osteochondrosis - disease of the spine, characterized by the degeneration of the intervertebral disc with a significant decrease in its height, sclerosing the disk surfaces of the vertebrae and the reactive growth of the edge osteophytes.
Content
Osteochondrosis damaged cloth discs gradually reborn and turns into a similarity of bone. The hardened disk decreases in size, loses the properties of the shock absorber between the vertebrae and begins to put pressure on the nervous endings, which leads to the appearance of painful sensations.
The initial stage of osteochondrosis most often does not show itself any unpleasant sensations in the spine and can be diagnosed as disease internal organs, and a true diagnosis is detected only after passing numerous surveys.
 Osteochondrosis is distinguished by osteochondrosis on, cervical, chest, lumbar, sacral and common osteochondrosis. Most often a lumbar osteochondrosis is diagnosed (over 50% of cases), cervical (more than 25%) and common (about 12%).
Osteochondrosis is distinguished by osteochondrosis on, cervical, chest, lumbar, sacral and common osteochondrosis. Most often a lumbar osteochondrosis is diagnosed (over 50% of cases), cervical (more than 25%) and common (about 12%).
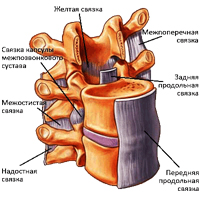
Intervertebral disc is a fiber-cartilaginous plate. In the middle of the disk there is a kernel, surrounded by a fibrous ring (fabric resembling tendons). The intervertebral disk does not have its vascular system and therefore feeds at the expense of other tissues. An important source of nutrients for the disk is the muscles of the back, it is their dystrophy most often leads to the development of osteochondrosis. When lifting weights, jumps and other exercise, discs perform the role of a shock absorber and support the required distance between the vertebrae. Since the largest load is to fall on the lumbar spine, it is in it that the protrusions and intervertebral hernia are most often formed, which are complicated osteochondrosis.
Protrusion of an intervertebral disc - Disk protrusion (prolapse) without breaking a fibrous ring.
The hernia of the intervertebral disc - protrusion (prolapse) of the disk with a breakdown of the fibrous ring and «leakage» centech kernel. Especially often, hernia is formed during the injury of the spine or during the simultaneous tilt and turning the body to the side, especially if there is heavy in the hands 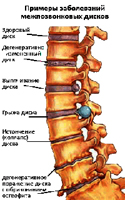 item. In this position, intervertebral discs are experiencing a very large load, the pressure inside the intervertebral disk rises, the vertebrae pressure on one side of the disk and the kernel is forced to shift in the opposite side and put pressure on the fibrous ring. At some point, the fibrous ring does not withstand such a load and the disk protrusion occurs (the fibrous ring is stretched, but it remains as a whole) or the hernia is formed (the fibrous ring is riveted and through a breakthrough «It follows» part of the kernel content). With an increase in the load on the spine and creating the conditions for increasing the pressure in the damaged incomplete disk of the hernia increases in size.
item. In this position, intervertebral discs are experiencing a very large load, the pressure inside the intervertebral disk rises, the vertebrae pressure on one side of the disk and the kernel is forced to shift in the opposite side and put pressure on the fibrous ring. At some point, the fibrous ring does not withstand such a load and the disk protrusion occurs (the fibrous ring is stretched, but it remains as a whole) or the hernia is formed (the fibrous ring is riveted and through a breakthrough «It follows» part of the kernel content). With an increase in the load on the spine and creating the conditions for increasing the pressure in the damaged incomplete disk of the hernia increases in size.
It is very important to the direction of the protrusion and the size of hernia, if hernia goes forward or to the parties, it can lead to pain and violation of the work of some organs, and when the spinal cord is protruding and damaged, the consequences may be much more serious. If the intervertebral hernia touched the nerve processes or roots of a certain spinal segment, this leads to a violation of the work of the body for which the damaged spine segment is responsible.
Another option is possible: due to the protrusion of the disk in one direction, in the opposite side, the distance between the vertebrae decreases and this leads to the pinch of the nerve processes by the vertebrae themselves. The intervertebral hernia in the lumbar department, most often causes pain in the legs, hernia in the chest contributes to the occurrence of dizziness, pain in the heart area, violations of the functions of the respiratory organs and T.D., hernia in the cervical department can cause headaches, dizziness, numbers.
Most dangerous intervertebral hernias The size of more than 10 mm, sharply narrowing the spinal channel, clamping blood vessels and injured nerve endings, long-term exposure to which leads not only to severe pain, but also to circulatory disruption, loss of sensitivity in limbs with subsequent complications.
But the most dangerous are sequential hernias of intervertebral discs, t.E. The hernia is ready for destruction or separation of a fragment with the subsequent lowering of it in the spinal channel, which can lead to severe consequences: violations of the functions of pelvic organs and paralysis of the lower extremities.
Causes of the disease
The reasons for causing changes in intervertebral disks were not fully understood. People begin to feel the manifestations of osteochondrosis most often after 35 years. The development and exacerbation of the spine osteochondrosis contributes to various injuries of the back, static and dynamic overloads, as well as vibration. The older man, the more manifestations of osteochondrosis. But in recent years, more and more people aged 18 to 30 years are treated with spin pain. The reasons for the early manifestation of the disease are a lot: weak physical training, violation of posture and curvature of the spine, flatfoot and excessive weight. And so, lay out The main reasons contributing to the emergence of osteochondrosis:
- Hereditary (genetic) predisposition;

- violation of metabolism in the body, infection, intoxication;
- overweight, improper nutrition (lack of trace elements and liquids);
- age changes;
- spinal injuries (bruises, fractures);
- Violation of posture, curvature of the spine, hypermobility (instability) of the spinal column segments, flatfoot;
- unfavorable environmental conditions;
- sedentary lifestyle;
- work related to lifting weights, frequent changes in the position of the body (turns, flexion and extension, jerk movements);
- The long-term exposure to uncomfortable poses in the standing position, sitting, lying, when lifting and transferring weights, when performing another work, in which the pressure in the disks is increased and the load on the spine as a whole;
- excessive physical exertion, unevenly developed kostomuscular system;
- spinal reloading associated with feet diseases, as well as as a result of wearing uncomfortable shoes, high heels and pregnancy in women;
- sharp cessation of regular training by professional athletes;
- nervous overvoltage, stressful situations, smoking;
- Supercooling, unfavorable meteo conditions (increased air humidity at low temperature).
Symptoms characteristic of osteochondrosis
Patients suffering from osteochondrosis are complaining of permanent backing back pains, which are often joined by numbness and feeling of fragmentation in the limbs. In the absence of adequate treatment, weight loss and limb atrophy occurs. The main symptoms of osteochondrosis are:
- constant backing pain in the back, feeling of numbness and lobs in the limbs;
- amplification of pain with sharp movements, exercise, lifting weights, cough and sneezing;
- Reducing the volume of movements, muscle spasms;
- With the osteochondrosis of the cervical spine: pain in hands, shoulders, headaches, it is possible to develop the so-called vertebral artery syndrome, which consists of the following complaints: noise in the head, dizziness, flashes «Mushhek», Colored spots in front of eyes in combination with burning pulsating headache. The cause of the vertebral artery syndrome can be its spasm in response to both the immediate irritation of its sympathetic plexus due to bone expansions, the hernia of the disk, the arrangement of the intervertebral joint, and the reflex reaction due to the irritation of any spinal receptor. The presence of a vertebral artery syndrome may aggravate the course of coronary or cardiovascular pathology if available;
- with osteochondrosis of the thoracic spine: the pain in the chest (as «count» in chest), in the field of heart and other internal organs;
- With osteochondrosis of the lumbosacral spine: pain in the lower back, irradiating in the crushes, the lower limbs, sometimes into the organs of the small pelvis;
- The damage to the nerve roots (in the hernias of intervertebral discs, bone growths, spondylolisthesis, spondyltroitrosis): shooting pain and sensitivity impairment, hypotrophy, hypotension, weakness in innervated muscles, reducing reflexes.
Diagnosis of osteochondrosis
Establishing a preliminary diagnosis is carried out with a primary examination of the patient. Inspection Usually conducts a neurologist in connection with the complaints of the patient for local changes, which can manifest themselves to painful syndrome, deformation or limitation of mobility. The spine is examined in the position of the patient standing, sitting and lying, both alone and in motion. The level of spine damage is determined by reference of the number of vertebrae from certain anatomical landmarks or by a special scheme.
In view of the backs pay attention to the posture, the features of the structure of the body, mark the line of spawn processes (the middle groove of the back), the lower corners of the blades, the ridges of the iliac bones, the side outlines of the waist and neck, the position of the adapter, the deviation of the intersective grooves from the vertical Pay attention to the muscle relief located next to the spine.
Spinal feeling allows you to supplement the inspection data (presence or absence of deformation), determine the localization, degree and nature of pain. When feeling, the tension of the muscles located next to the spine, T.To. Most injuries and diseases of the spine are accompanied by an increase in muscle tone.
The flexion of the spine is used to determine the amplitude of movements in various spinal deposits.
The main role in the study of the spine is removed radiography, computer tomography and magnetic resonance imaging, with which the level of lesion is determined, and the diagnosis is specified, hidden pathologies are revealed. Diagnostic data allow the doctor to determine the treatment tactics and choose the most effective methods of treatment.
Methods for treating osteochondrosis and its complications
 The treatment of osteochondrosis and its complications are carried out with the help of conservative methods aimed at eliminating pain syndrome, violations of the function of the spinal roots and the prevention of the progression of dystrophic changes in the spinal structures. With the ineffectiveness of conservative treatment and according to special indications, operational (surgical) treatment is carried out, the volume of which depends on the level of damage and clinical manifestations of the disease.
The treatment of osteochondrosis and its complications are carried out with the help of conservative methods aimed at eliminating pain syndrome, violations of the function of the spinal roots and the prevention of the progression of dystrophic changes in the spinal structures. With the ineffectiveness of conservative treatment and according to special indications, operational (surgical) treatment is carried out, the volume of which depends on the level of damage and clinical manifestations of the disease.
The duration of treatment of osteochondrosis and its complications mainly depends on the severity of the disease, age-related changes applied methods of treatment, as well as the conscientious fulfillment of appointments and recommendations of the attending physician. As practice shows, the active phase of treatment in most cases lasts 1-3 months when applying conservative methods, and the recovery period after the operation is about 1 year.
At the beginning of treatment, some patients are able to enhance pain syndrome associated with the reaction of the muscular system and other formations for unusual impacts for the body. Paints are stopped in a short time using physiotherapy procedures, drugs, as well as special exercise. The result of treatment largely depends on the behavior of the patients themselves, from which patience, perseverance, perseverance, a certain power of will, as well as the desire to recover. The greatest effectiveness of conservative therapy and rehabilitation after surgery can be achieved in the conditions of specialized medical centers and sanatoriums equipped with a modern diagnostic and therapeutic base, as well as highly qualified practitioners using a comprehensive treatment of diseases of the musculoskeletal system.
Complex conservative treatment includes Medical physical culture, physiotherapy, massage, manual therapy, stretching (traction) of the spine, reflexotherapy, drug therapy.
Medical Physical Culture (LFC) - The main method of conservative treatment of diseases of the musculoskeletal system is to create dosage loads aimed at decompression of nerve roots, correction and strengthening of a muscular corset, an increase in the volume and generation of a certain stereotype of movements and the correct posture, giving the binder muscular apparatus the necessary flexibility, as well as Prevention of complications. This is achieved by regular exercises on rehabilitation equipment and articular gymnastics. As a result of the exercise, the blood circulation is improved, the metabolism and power supply of intervertebral disks is normalized, the intervertebral space increases, a muscular corset is formed and the load on the spine is reduced.
Physiotherapy - Treatment method in which physical factors are used: low frequency currents, magnetic fields, ultrasound, laser, etc. Used to remove pain syndrome, inflammatory processes, rehabilitation after injuries and operations. When using physiotherapy methods, the treatment of many diseases is reduced, the efficiency of the use of medicines and the reduction of their dosage increases, there are no side effects inherent in drug treatment.
Massage - This set of techniques of mechanical dosage effects in the form of friction, pressure, vibrations carried out directly on the surface of the human body with hands. Effectively removes muscle tension, muscle pain, improves blood circulation, has a lining effect.
Manual therapy - Individually selected manual impact on the bone muscular system for removing acute and chronic pains in the spine and joints, as well as increasing the volume of movements and correction of posture. One of the directions of manual therapy is visceral manual therapy, which contributes to the restoration of normal organ mobility, improves blood supply, lymphocyerculation, normalizes the metabolism, restores immunity, prevents exacerbations of chronic diseases.
Pulling (traction) of the spine - Effective method for the treatment of pain syndromes in the spine, and joints using individually selected load using special equipment. The procedure is aimed at increasing the intervertebral space, the removal of pain and the restoration of the anatomically correct form of the spine.
Reflexology - Various therapeutic techniques and methods of impact on the reflexogenic zones of human body and acupuncture points. Application of reflexology in combination with other healing methods, significantly increases their effectiveness. The most often reflexology is used in osteochondrosis, accompanied by pain syndrome, diseases of the nervous system, sleep disorders, mental impassions, as well as overweight and tobacco. Impacting on certain points can be given a body into harmony and treat many diseases.
Drug therapy is shown during the exacerbation of the disease, aimed at relieving pain syndrome, removing the inflammatory process and enhancing metabolic processes by taking or administering medicines using intramuscular or intravenous injections. Although each of the above methods is highly efficient, still a persistent therapeutic effect can only be obtained when they are combined with exercises in rehabilitation equipment, T.E. When creating a full-fledged muscular corset.
Recommendations for the prevention and prevention of osteochondrosis
For the prevention of osteochondrosis or reduce pain people suffering from this disease, it is recommended that as many time as possible is in this position, in which the load on intervertebral discs is minimal, and at the same time, it is necessary to intimidate the back muscles as much as possible maintain exchange processes around the spine. General recommendations are reduced to compliance with the rules of a healthy lifestyle, in addition, in each particular case, the attending physician determines and private recommendations.
For the prevention of osteochondrosis, the following rules should be followed:
Do not overload the spine, do not create conditions contributing to the increase in pressure in intervertebral disks:
- Limit vertical loads;
- Do not make sharp movements, especially turning the body when the slope;
- Avoid drops and jumps from a high height, injuries and spinal bruises;
- more often change the position of the body;
- Keep your back smoothly;
- Try to keep the natural physiological bends of the spine: in the position of the lying, the load on the spine is minimal, but the bed must be a half rider (it is advisable to sleep on a solid orthopedic mattress and an orthopedic pillow); in a position sitting back to keep smoothly at the expense of the muscles or pressing it to the back of the chair or chairs. (The seat must be rigid enough, and the back has bending in the loaf area), keep your head straight; in the standing position more often change the leg to which you rely; get up from bed or from the chair, and also go to bed and sit, it should be not tightening with hands and not bending your back;
- Before physical load, drink water and massage the back, it will turn away blood, accelerate the metabolic processes and will allow the intervertebral discs to absorb a sufficient amount of moisture;
- Do not lift and do not hold heavy items on the elongated hands, to raise the item, sit down, and then get up with it, and the items should be as close as possible to the body;
- When carrying weights, try to evenly distribute the load, that is, do not wear bags in one hand and t.D., If you have to bear the subject in front of you, keep it as closer to the body, and, passing it, do not pull your hands forward, and also use for carrying weights of the cart, bags or suitcases on wheels, backpacks;
- When performing heavy work associated with lifting, movement or carrying weight, use a wide belt or special corset;
- For persons suffering from osteochondrosis, load more than 10 kg;
- When performing any work, try to be touched as much as possible and be in a bent state and periodically unload the spine (VIS on the crossbar, squeezing with the rise of the hands, rest lying);
- Wear comfortable shoes, women should limit walking in high-heeled shoes;
Regularly perform exercise aimed at strengthening and maintaining a muscular corset. Useful swimming classes.
Take a contrast shower, harden the body.
Do not overcoat.
Avoid scandals, stressful situations.
Clear correctly.
Do not smoke.
Complex of exercise for independent activities
The complex is intended for the prevention of osteochondrosis of various spinal departments. Daily performance of exercise will help strengthen the muscles, keep the spine flexible and movable. The complex serves as an addition to regular classes by forceful exercises aimed at strengthening and maintaining a muscular corset.
Exercise for the cervical spine:
- Put the forehead on the palm and strain the muscles of the neck. Exercise Perform 3 times to 7 seconds. Then put on the palm of the back and also 3 times to 7 seconds.
- Tension the muscles of the neck, press the left temple on the left palm (3 times to 7 seconds), and then right-wing visits put on the right palm (3 times to 7 seconds).
- Head slightly back. Overcoming the resistance of the tense muscles of the neck, press the chin to the tier. Perform an exercise at least 5 times.
- Hold your head and shoulders straight. Slowly turn the head to the right to the right (5 times). Some times do the movement to the left.
- Chin drop to the neck. Turn the head first 5 times right, and then 5 times left.
- Back head back. Try to touch the right ear of the right shoulder (5 times). Perform this move, trying to touch the left shoulder to touch the left shoulder (5 times).
Exercise for the thoracic spine:
- AND.NS. - Doing inhale, stand straight, hands down, legs together. Pull the hands up - exhale. Rock back and take a deep breath. Then lower your arms, lean forward, slightly rounded back, lower your shoulders and head - exhale. Repeat 8 - 10 times.
- AND.NS. - Sitting on a chair. Get your hands behind the head - inhale, get downloaded back 3 - 5 times, leaning the blades about the back of the chair - exhale.
- AND.NS. - Stand on all fours. Get your back as much as possible and hold for 2 to 3 seconds in this position. Hold your head right. Holy breathing. Repeat the exercise 5 - 7 times.
- AND.NS. - Lie on the stomach and assume your hands in the floor. Rock up the most, trying to tear the body from the floor. Holy breathing. Repeat the exercise 5 - 8 times.
- AND.NS. - Lying on the stomach, hands along the body. Dock in the thoracic spine, trying to raise the head and legs as much as much as possible. Holy breathing. Repeat the exercise 5 - 8 times.
Exercise for the lumbar spine:
- VIS or semi-suite for 70 seconds. on the crossbar that you can kill above the door.
- AND.NS. - standing hands on hips. Tilting forward, back, right, left. Repeat 10 times in each direction.
- AND.NS. - standing hands on hips. Movement of the pelvic forward, back. Repeat 10 times in each direction.
- AND.NS. - standing on the knees, stopped with straight hands in the floor. Work out like a perochny knife, then return to its original position. Repeat 15 - 20 times.
- AND.NS. - lying on the stomach, stopped bent hands in the floor. Straighten your hands, squeeze the floor, without taking off the legs. Repeat 10 - 15 times.
- AND.NS. - standing on the knees, stopped with straight hands in the floor. Get back the back up, go back in and.NS. Repeat 10 - 15 times.
- AND.NS. - Lying on the back. Press the legs bent in the knees to the chest. Repeat 10 - 15 times.
Recommendations for patients who have undergone an operation to remove the hernia of an intervertebral disk
The rehabilitation process takes from 3 months to 1 year after the operation, depending on its complexity. After 6 months, patients are recommended to continue classes on rehabilitation equipment under the control of the doctor's physician or instructor in order to prevent the recurrence of the hernia of an intervertebral disk, for which a complex of exercises is individually selected for creating a muscular corset and improving blood circulation in problem areas.
The recovery period is under the supervision of a neurologist's doctor who appoints a course of drug therapy, recommends consultations of other specialists for more effective treatment.
The recovery period is under the supervision of a neurologist's doctor who appoints a course of drug therapy, recommends consultations of other specialists for more effective treatment.
Early rehabilitation period (from the 1st to 3 months).
Recommendations:
- Do not sit for 3-6 weeks after surgery (depending on the severity of the operation).
- Do not make sharp and deep movements in the spine, tilts forward, on the sides, twisting movements in the lumbar spine within 1-2 months after surgery.
- Do not get behind the wheel and not ride in transport in the sitting position within 2-3 months after surgery (you can ride as a passenger half-round, laying out the seat).
- Do not lift more than 3-5 kilograms for 3 months.
- Within 3 months after the operation, do not follow a bike, engage in sports sports (football, volleyball, basketball, tennis and t.D.).
- Periodically unload the spine (rest in the position lying for 20-30 minutes during the day).
- Wearing a postoperative corset not more than 3 hours a day.
- It is advisable not to smoke and not drink alcohol during the entire period of rehabilitation. Intimate life is not contraindicated.
Rehabilitation:
As soon as the patient is allowed to walk, it should consult with the physical physical physics on the timing of the appointment and a complex of therapeutic physical education, which depend on the volume and nature of operational intervention, as well as postoperative complications. A month after an uncomplicated operation, classes in the gym (not in the simulator!) under the control of the physician exercise, without turning loads. Useful swimming on the stomach.
A month after the operation in uncomplicated cases, it is possible to start work (the question of terms and specifically performed work is solved in each case individually with the attending physician).
Late rehabilitation period (3-6 months).
Recommendations:
It is not recommended to raise more than 5-8 kilograms, especially without warm-up and heating of the muscles of the back, jumping from the height, long trips by car.
When exiting the street in bad weather: wind, rain, low temperature, it is desirable to wear an insulation belt to the lower back area.
Wearing a corset, especially long, is not recommended to avoid atrophy of the long muscles of the back.
Rehabilitation:
In this period, you can carefully under the control of the physician LFC to start the formation of a muscular corset, engaged in exercises to strengthen the muscles of the back.
After 6 months and at least 2 times a year it is recommended to undergo a course of massage, physiotherapy and gentle manual therapy for all spine departments.
Healthy lifestyle, rejection of smoking, regular classes in the gymnastic hall, swimming, bath, limit lifting weights significantly reduce the risk of gnage of intervertebral disks.
For the prevention of back pain should be avoided: stress, supercooling, long monotonous labor in a forced pose, lifting weights, sharp movements on cold, not preheated muscles, appearance of overweight body.
In addition, at any stage of rehabilitation, it is possible to include in a complex of rehabilitation measures in needleflexotherapy and physiotherapy.









