Intervertebral hernia and intervertebral disk protrusion are hazardous complications of the degenerative process in intervertebral disks - spinal osteochondrosis. The earlier diagnose the intervertebral hernia, the more likely to avoid its complications and fully restore the patient's health.
Content
Intervertebral hernia — This disease of the spine caused by injury, lifting weights, or the resulting effect of idiopathic factors, in which, as a result of a fibrous ring gap occurs «Digging» Soft central part of an intervertebral disk (pulp nucleus) beyond the damaged fibrous ring. Gaps almost always have rear agent (back and lump) character, which is associated with the presence of the rear longitudinal bunch in the spinal channel.
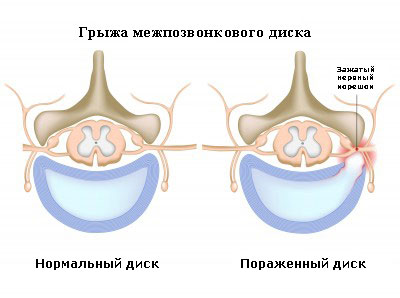
In acute development of intervertebral hernia, the discrepancy of the fibrous ring can lead to the activation of chemical mediators of inflammation, which in itself causes severe pain, even in the absence of a stress of the nervous root. Most often, the intervertebral hernia is one of the complications of the complex degenerative disease of the spine, osteochondrosis, mainly affecting intervertebral discs. Due to the power disorders, discs lose their elasticity, cease to perform the function of shock absorbers, become vulnerable to any mechanical effect. This state of intervertebral discs is a powerful risk factor for occurrence «protrusion» Pulpous kernel (protrusion or hernia of an intervertebral disk). That is why in the treatment of intervertebral hernia and protrusions, it is necessary to take into account the overall state of intervertebral discs and a complex of medical and preventive procedures aimed not only to reduce hernia formations, but also to the improvement of the entire spine.
Most often, intervertebral hernias occur in the lumbar spine (95% in L4-L5 or L5-S1), the cervical (C5-C6, C6-C7) is a little less. Hernia and prudrusions of the chest are rare. In all cases, symptoms are similar, although pain syndrome, sensory and motor disorders and have different localization.
Anatomy
Our spine consists of 32–34 bones called vertebrae. These bones create a canal that protects the spinal cord. Severate five spinal departments:
- cervical (7 vertebrae, C1-C7);
- thoracic (12 vertebrae, TH1-TH12);
- Lumbar (5 vertebrae, L1-L5);
- sacral (5 vertebrals, S1-S5);
- Copchik (3-5 vertebrae, CO1—CO5).
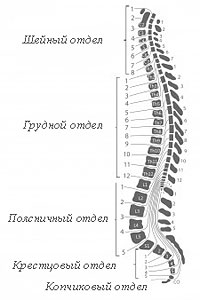 5 sacral bones in adulthood spliced, forming the crushes, and the smoking department (or the tailbone) of a person consists of three-five surrounding rudimentary vertebrae. The last intervertebral disk is located between the last lumbar vertebra (L5) and the first sacral (S1).
5 sacral bones in adulthood spliced, forming the crushes, and the smoking department (or the tailbone) of a person consists of three-five surrounding rudimentary vertebrae. The last intervertebral disk is located between the last lumbar vertebra (L5) and the first sacral (S1).
There are spinal cords and nerves in the spinal canal. These «Electrical cables» tolerate pulses from the brain to the muscles.
Intervertebral discs — Elastic interlayers located between the vertebrae. They perform the function of shock absorbers when we go or run.
Intervertebral discs are flat and round fibrous-cartilaginous formations and consist of two parts: a fibrous ring (rigid flexible disk outer shell) and a pulp nucleus (soft jelly disk center).
As we have already found out, the bones of the spinal column protect the nerves coming out of the brain and descending down the spine. These nerves form a spinal cord. Nervous roots — These are large nerves that branched out the spinal cord and leave the vertebral pole between the vertebrae.
The vertebrae is divided among themselves with intervertebral discs. Intervertebral discs soften friction between the vertebrae and provide flexibility and depreciation of the spine.
Intervertebral discs can be shifted («Spent») or break during damage or deformation. In this case, pressure may occur on the nerves of the spine. The grinding of nerves is the cause of pain, numbness and weakness.
Lower Spinal Department (lumbar region) is amazed most often. Intervertebral discs of the cervical department suffer much less. The hernia of the thoracic spine is extremely rare.
Radiculopathy — This disease affecting nervous roots. The hernia of the intervertebral disk is one of the causes of radiculopathy.
Factors increasing the risk of an intervertebral disk hernia:
- Age. The hernia of the intervertebral disk is more common in middle-aged people (35-45 years). This is due to age degenerative changes in the spine.
- Excess weight. Big body weight increases the load on intervertebral discs.
- Work related to lifting weights, as well as power sports.
- A sedentary lifestyle, conjugate with a constant static load on the spine, also contributes to the emergence of osteochondrosis, hernia and protrusions of intervertebral disks.
- Weight loss as a result of unbalanced diets and hunger strikes effect on the exchange processes of the whole organism, including disturbing the power of intervertebral disks, which leads to the emergence of dystrophic disease of the spine (osteochondrosis).
- Smoking. Scientists have proven that smoking increases the risk of osteochondrosis and, as a result, intervertebral hernia and protrusions.
- Congenital spinal defects and spinal column. For example, Shayerman-Mau's disease («Wedge-shaped» vertebrae).
Symptoms of intervertebral grozhi
 The symptoms of the hernia of the intervertebral disc vary from the lungs of the pulsating pain. In some cases, pain is so strong that the patient cannot move. Typically pain is localized on one side of the body.
The symptoms of the hernia of the intervertebral disc vary from the lungs of the pulsating pain. In some cases, pain is so strong that the patient cannot move. Typically pain is localized on one side of the body.
In the hernia of the lumbar spine in the patient, an acute pain may occur in some parts of the leg, hips or buttocks and numbness in other areas. It can also feel pain or numbness on the back of the tibia or in the foot. Weak may be felt in the same leg.
For hernia, the cervical spine is characterized by pain in the neck when turning the head, acute pain in the shoulder or in the field of blades, as well as pain, irradiating in hand, forearm and (less often) fingers. Also frequent symptoms are numb in shoulder, in the elbow, forearm and fingers.
Usually the pain is enhanced:
- After you got up or sat down,
- at night,
- when sneezing, cough and laugh,
- During a long walk.
Patients often complain of weakness in some muscles. Sometimes muscle weakness is detected only with neurological examination, but it happens that the patient himself feels that he is hard to lift his leg or hand, stand on socks, compress the fingers of one hand into the fist.
Neurological examination
Conducting a thorough neurological inspection is necessary for the diagnosis and appointment of adequate treatment. Relying on the patient's complaints, the doctor conducts a neck examination, shoulders, hands and hands or waxes, hips, feet and stop.
Neurological examination includes:
- Detection of the area of numbness or loss of sensitivity,
- Checking muscle reflexes that can be slowed down or fall out at all,
- assessing muscular power,
- Detection of violations of posture.
The doctor may also ask:
- sit down, stand up or walk. While walking, he may ask to walk first on the heels, and then on socks,
- lean forward back or sides,
- Tilt the neck back, back or sides,
- lift shoulders, wrist or hand and check their muscle strength.
Pain in the leg arising when you sit on the couch, and raise your leg up, usually speaks of damage to the lumbar spine.
During another test, the doctor may ask to tilt his head forward or to the sides, while pressing the top of the head. Strengthening pain or numbness during the test will talk about squeezing the nerves of the cervical spine.
Neurological inspection allows you to put a preliminary diagnosis and send a patient to a spinal survey. At the moment, the most progressive method for identifying hernia or protrusions of intervertebral discs is magnetic resonance tomography (MRI).
We recommend to carry out magnetic resonance imaging only on high-polished devices with a magnetic field strength of at least 1 Tesla.
Treatment with intervertebral hernia is prescribed depending on its size, the remainder of the fool bag after hernia, the number of intervertebral hernias and protrusions, the severity of other complications of osteochondrosis — Spondidalese and spondyloarthrosis. In most cases, with intervertebral hernia, it is possible to provide effective assistance without surgery.