Terrible pain around the body does not give neither sigh... Over the past 30-35 years, diagnosis «osteocondritis of the spine» became known to many. Osteochondrosis is the gradual destruction of the vertebrae, and the intervertebral hernia - its complication. Our article on intervertebral hernias and their treatment according to the method of Dr. Solomatova.
Content
Intervertebral cartilages are elastic springs, gaskets between vertebrae, capable of flattening and then restore their original shape. The physiological meaning of this is the preservation of some fixed space between adjacent vertebrae, in order for the spine to make movements in different directions, but at the same time remained in the former anatomical boundaries and relations.
Intervertebral cartilage has a complex structure. The inner elastic part (pulpbogenous kernel) is surrounded by a so-called fibrous ring, a cloth in physical parameters resembling tendon.
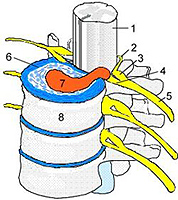
If the cartilage is flattened from squeezing between the vertebrae, but the fibrous ring is not broken, such a state is called «Prolapse», «Protrusia», T.E. «Protecting». If the cartilage is flattened to such an extent that the fibrous ring does not withstand pressure from the inside, and is broken, and the internal contents of the cartilage falls out into this gap, just such a state and is the hernia of intervertebral cartilage (cm. drawing: one - spinal cord; 2 - rear root; 3 - spinal gagli; 4 - Mudka vertebra; five - spindose nerve; 6 - intervertebral disk; 7 - hernia; eight - vertebral body). By the size of the catastrophe, the occurrence of the hernia of intervertebral cartilage can be compared with the bone fracture.
The danger of the hernia of intervertebral cartilage, in addition to the pronounced overall impact, the condition of a person, its social status, long-term exhausting pain, is possible its impact on the nerve tissues or vessels that feed the spinal cord. At the first stage of their appearance, it depends on:
one. Directions of extrusion cartilage. Cartilage, squeezed to the spinal cord or transmission vessels, blood supplying spinal cord, much more dangerous hernia, crushed forward or sideways.
2. The level of appearance of the hernia. Hernia in the spine departments through which the spinal cord passes much more dangerous for possible consequences than hernia in the lumbar section, below the 1-2rd lumbar vertebrae, that is, below the end of the spinal cord.
Then, even at the time of its appearance, the nerve fabric immediately did not destroy the nerve fabrics, the further deterioration of the person's state (up to paralysis, a sudden death in a dream due to the stopping of breathing - with hernias in the cervical spine) may occur due to:
-
Further increase in the size of the untreated hernia, because the root causes of the destruction of the ligaments are not eliminated. Bone corn is absent, t.E. Herry Gate remain open and hernia at any time can continue their movement towards the nervous tissue.
-
Manipulation T.N. «manual professionals». It is clear that if any intervertebral hernia is cartilage extruded through broken ligaments, and manual therapy techniques often lead to additional stretching of the gaps of breaks, cartilage can continue their movement, up to full loss of intervertebral space. The consequences of this are unpredictable, especially with hernias in the cervical department, up to the subsequent fatal.
-
Incorrect or intense exercises during exacerbation periods. The mechanism is approximately the same as when exposed «manual professionals», But in these cases, the movements committed by the person may lead to stretching torn ligaments.
-
Conducting unreasonable surgical operations. As a result, the emergence of intervertebral hernia is provoked, or even one, above or below the operated location. In recent years, in the terminology of surgeons to designate the weakening of the spine, the rotation of the nerve endings and nerves into the scar, which necessarily arises after removing the echo tissues around the intervertebral hernia, the term appeared - «Operated spine syndrome».
 «The more you take, the more it becomes…»
«The more you take, the more it becomes…»
Re-emerged pain (usually in time from several months to 2-4 years, if you are lucky) in this case, it is precisely the rotation of the nerve tissues into the scar and is no longer amenable to any medicine, except for re-excision of the scar, t.E. Operations leading to the final destruction of the nerve. As in the riddle about the pit: «The more you take, the more it becomes…». Only the validity of terrible in the final results - exchange, trophic disorders in controlled tissues, vascular disorders, continuing pain in the spine and limbs, increase blood pressure within 4-5 years after the operation, and many other complications.
Indications for the operational treatment of the hernia of intervertebral cartilage (all the more urgent), contrary to zealous statements of neurosurgeons, very little. The only, but not always binding, indications for the operation are the above-mentioned signs of squeezing the spinal cord or vessels that feed the spinal cord, namely:
-
Paraliacy, Parese. Their manifestations are muscular weakness and reduction of muscles in size (without pronounced pain).
-
Disorders of nervous control over the work of the pelvic organs that are manifested by the inability to overcome or involuntary urination, the impossibility of conscious control over the activities of the rectum - involuntary defecation.
During the reference of the decision to conduct a surgical operation - necessary for these few life indications - it should always be borne in mind that the higher the 1st lumbar vertebrae the level of hernia appearance, the more dangerous not only the hernia itself, but also the consequences of the operation on the spine. Up to the deadly outcome on the operating table during operations in the cervical.
All other manifestations of intervertebral hernia: severe pain, reduced sensitivity, weakness of muscles from inaction (due to the fact that the movement causes pain), changes of reflexes and T.D. - disappear after the disappearance of edema and sinking of hemorrhages in the intervertebral hernia zone. All these phenomena are frequent in patients with «ordinary», not complicated osteochondrosis of the spine - without intervertebral hernia.
In addition to the treatment of the osteochondrosis of the spine, the therapeutic impact on systems regulating calcium exchange in the body is always added. By analogy with the treatment of the bone fracture, it is also necessary to speed up the healing of the fracture site, and to do so, accelerate the deposition of calcium salts to the place of the gap, in order for it «Oaksenelo» (bone corn formed) so that the adjacent vertebrae comes together. This is the only way to eliminate forever and prevent squeezing cartilage in this place.
Another direction of therapeutic effects is the stimulation of cellular immunity - phagocytosis. There are special cells in the body - phagocytes that purify the body from non-viable tissues (absorb, «devouring» Dead, unnavatic or foreign fabrics). Their activity depends on the condition of the liver and the large intestine. The correction of the work of these organs stimulates the activity of phagocyte cells. Thanks to their activities, the chuck disappears, is resolved.
For stimulation of recovery processes, point vibration reflexotherapy and the impact of plant, metal and other stimulants are used.