With this disease, the immune system, which is normally struggling with foreign microorganisms and substances, as if «breaks down» and begins to destroy his own cells. So arise autoimmune diseases to which red lupus belongs to.
Content
The leather, heart, lungs, kidneys, joints and nervous system affect the red lupus. If only skin is affected, such a disease is called Discoidal Red Volcanka. If the process involves internal organs, the disease is called systemic red lupus, or SC.
Both types of lupols are 8 times more common in women than men. The disease can begin at any age, but most often it takes place between 20 and 45 years.
The reason causing lupus is unknown. Obviously, heredity, viruses, ultraviolet radiation and some drugs play a certain role. It is assumed that the immune system in patients with a red lupus genetically more susceptible to the effects of external factors, such as viruses and ultraviolet radiation.
Volchanka can cause several dozen drugs, but in more than 90% of cases, medicinal lupus develops after taking six drugs: hydralazine (preparation for hypertension), quinine and procainamide (used for treatment of arrhythmias), phenyotine (epilepsy treatment), isoniazide (tuberculosis treatment ), Dr. Penicilline (treatment of rheumatoid arthritis). Medicinal lupus, fortunately, occurs quite rarely and passes independently after stopping the reception of the drug.
It is known that some women have the flow of lupus worsen during menstruation. This phenomenon, as well as the predominance of women among the diseases, shows that women's sex hormones play a certain role in the development of lupus.
How does the red lupus manifest?
Discoidal lupus: rash with a discoid lupus has a red color, does not cause pain and itch. In 5-10% of cases, discoaded lupus (isolated lesion of the skin) goes into a systemic (damage internal organs).
When SLE meet various combinations of symptoms. The most frequent complaints: weakness, low temperature, loss of appetite, pain in the muscles and joints, ulcers in the mouth, rash on the face (in shape «Butterfly»), increased skin sensitivity to light, inflammation of the lung shell (pleurisy) and hearts (pericarditis), violation of the blood supply of fingers and legs under the influence of cold (the so-called Riino phenomenon).
Rash on her face. Develops approximately half of the halves of red lupus. It occurs on the nose and under the eyes - the so-called «butterfly». This rash is painless, does not cause itching, can increase under the influence of sunlight.
Arthritis. Develops sooner or later in most patients. Arthritis at the Volchanka is characterized by swelling, pain, stiffness and deformation of the joints of the brushes and stop. In some cases, the defeat of the joints at SLE reminds the defeat of the joints in rheumatoid arthritis. Sometimes there are inflammation and pain in the muscles (myositis).
Vasculit, or inflammation of blood vessels. Leads to a violation of blood supply to various organs and tissues.
Purit and pericarditis. Inflammation of the shell of lungs and hearts, respectively. Causes acute chest pain, which is intensified with deep breath, cough and changing body position. The defeat of the muscles of the heart (carditan) and heart valves (endocarditis).
Nephritis. When the sk is often affected by the kidneys, this complication is called a lupus jade. In nephrite, protein appears in the urine, blood pressure increases. Milk nephritis can lead to renal failure, when a kidney change is required to maintain the patient's life, or conduct dialysis (connection to the machine «Artificial kidney»).
Changes in psyche. Due to involvement in the pathological process of the brain in patients with SLE, there may be a change in personality, the development of psychosis, convulsions and even coma. Brain defeat is called cerebrit. The pathological process in the peripheral nervous system can lead to the loss of functions of individual nerves - it causes weakness of certain muscle groups, numbness and loss of sensitivity in those places that «serve» affected nerves.
Alopecia. Many patients with lupus fall out hair, this process is called alopecia, its activity often coincides with the overall activity of the disease.
In patients with lupus, a wide variety of symptoms can be observed, so eleven diagnostic criteria were developed to facilitate the diagnostic criteria - the characteristic symptoms of lupus. If there are four or more criteria, the diagnosis of lupus is considered «Very likely». In some patients, not all criteria are manifested immediately, others - for all the time there are only 2-3 criteria.
 Criteria of the American Rheumatic Association:
Criteria of the American Rheumatic Association:
In addition to these eleven criteria for diagnosis, some other tests are used, for example, e /e, biochemical analyzes, tissue biopsy and t.D.
Cure SLE completely impossible. The purpose of treatment is to facilitate the symptoms, protect organs and tissues from our own immune system, reduce inflammation and autoimmune process.
Nonteroidal antiber drugs (NSAIDs) reduce inflammation and pain in muscles, joints and other tissues. The NSAID group includes aspirin, ibuprofen, naproxen, Voltaren, Sulindak and DR. Source effects of NSAIDs: irritation of the gastric mucosa, the development of gastritis and ulcers (therefore, these drugs must be taken after meals), reduced blood coagulation.
Corticosteroids have a stronger anti-inflammatory action than NSAIDs. Corticosteroids can be taken in tablets, introduce in injections to joints or intravenously. Unfortunately, corticosteroids have many serious side effects, especially when they are used for a long time in large doses.
The most common side effects: obesity, osteoporosis, infection, diabetes, cataract, necrosis of large joints, enhancing arterial pressure. To reduce the severity and frequency of side effects of steroids try to prescribe in minimal doses.
Hydroxychlorocavine (PLAKVENIL) - antimaryary preparation, which is particularly effective in patients with SLE with weakness, lesion of the skin and joints. Hydroxychlorocavine reduces the frequency of thrombosis, especially against the background of the presence of the so-called antiphospholipid syndrome. Side Effects: Diarreya, Stomach Disorder, Pigment Eye Changes (Therefore, treatment should be carried out under the control of ophthalmologist).
Immunosuppressors - drugs that overwhelming the immune system. These drugs are used in the severe clock of the lupus, when the disease amazes internal organs. The immunosuppressors include methotrexate, azathioprine, cyclophosphamide, chlorambucil and cyclosporine.
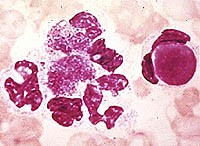
All these drugs can cause the drop in the number of erythrocytes, leukocytes and blood platelets, which leads to anemia, frequent infections and bleeding. There are other side effects, for example, methotrexate toxic to the liver, and cyclosporin - for kidneys. Immunosuppressors can only be used under the strict control of the rheumatologist, with regular surrenders.
How to avoid aggravations of lupus?
SLE - severe disease affecting many organs that can lead to invadillating and even death. Nevertheless, it is important to understand that patients with SLE can live a normal active life, especially during remission. And the exacerbations of the disease should be made medicine.
Ultraviolet irradiation can cause an aggravation or worsening its course of the disease, so patients with a lupus should avoid staying in the sun, if necessary - use long sleeves and sunscreen clothing.
Patients should be accurately taken to take prescribed drugs and in no way interrupt corticosteroids sharply - it can provoke exacerbation.
Patients with SLE, especially if they take corticosteroids or immunosuppressors are subjected to increased risk of infections, so patients need to immediately inform the doctor about any increase in temperature.
One of the conditions for successful treatment of SLE - constant contact between the patient and the doctor. The doctor should be aware of the changes in the health state of the patient, the appearance of new symptoms, the side effects of drugs and T.D.
Pregnancy in a patient with SLE refer to category «High risk». The patient's entire pregnancy should be observed with a rheumatologist and an obstetrician, since the risk of miscarriage in such patients is very high, especially in the presence of so-called phospholipid antibodies (cardiolipin antibodies, a solid anticoagulant).
Phospholipid antibodies cause a tendency to thrombosis, so aspirin is often prescribed (sometimes together with heparin) in order to «Light» blood. Some specialists in particular testimony are also prescribed immunoglobulin
Wolves antibodies can be transmitted from mother to child, as a result develops «Magician newborns», characterized by decreases of erythrocytes, platelets and leukocytes in the blood of a baby, the appearance of skin rash. In some newborns, the blockade of the heart (violation of electrical impulses in the heart) - in such cases, consultation of the cardiologist is required.
Lupils of newborns more often occurs if the mothers are detected by anti-RO (SS - A) and anti-La (SS - B) of antibodies - the risk of the development of lupus in the infant in this case is 5%, and the risk of developing the blockade of the heart - 2%. Usually, lupus newborns runs in about 6 months, when maternal antibodies in the child's body are destroyed.










