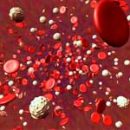
Agranulocytosis is also called deep leukopenia, because for this disease is characterized by a very sharp drop in the number of leukocytes, and sometimes their complete disappearance. More about agranulocytosis and its forms - read the article.
Content
 Agranulocytosis is characterized by a sharp decrease or absence in peripheral blood grainy leukocytes. Single cases of this disease were described back in 1907 by Turk, and in 1922, Schulg gave him a detailed clinical and hematological characteristic and the name of agranulocyte angina. Schulg considered characteristic of this disease, the presence of necrotic angine or necrotic foci on mucous membranes, high temperature and sharp decrease in the number of leukocytes (2-1) g / l with relative lymphocytosis - up to 80-90% and a sharp decrease in almost decrease in granulocytes.
Agranulocytosis is characterized by a sharp decrease or absence in peripheral blood grainy leukocytes. Single cases of this disease were described back in 1907 by Turk, and in 1922, Schulg gave him a detailed clinical and hematological characteristic and the name of agranulocyte angina. Schulg considered characteristic of this disease, the presence of necrotic angine or necrotic foci on mucous membranes, high temperature and sharp decrease in the number of leukocytes (2-1) g / l with relative lymphocytosis - up to 80-90% and a sharp decrease in almost decrease in granulocytes.Women suffer agranulocytosis more often than men, children less often than adults.
For reasons that determine the development of the disease include infections, sepsis, tuberculosis, abdominal title, leukemia growth, cancer metastases and other malignant neoplasms in the bone marrow, as well as the use of medicines, ray energy action, cytostatic (antitumor) treatment.
According to the mechanism of development, 2 forms of agranulocytosis are isolated - immune and myelotoxic.
The antigen reaction - the antibody passes in the presence of the Hapten (fragment of the biopolymer molecule or artificially synthesized chemical compound), the role of which is most often performed by medicines. Agranulocytic antibodies show their action first in peripheral blood, the result of which is the death of mature neutrophilic granulocytes, and then more young granulocytes located in principle to the precursor cells of the granulocyrtic row in the bone marrow.
The development of this form of agranulocytosis is the body's response in response to the reception of one or another medication. There are many different medicines that can contribute to the development of immune agranulocytosis. These include: amidopin, butadion, fenacetin, etc.
It should be remembered that chemical and medicinal substances depending on the mechanism of action can cause myelotoxic in some cases, and in the second - immune agranulocytosis.
Medicinal agranulocytosis is observed by acute start with an increase in temperature to 38-39O, the appearance of angina, stomatitis, with development in some cases of the oral mucosa, larynx and esophagus.
Changes in peripher blood depend on the severity of the disease.
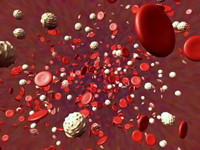
Characterized increasing leukopenia (up to 1-3 g / l) by reducing the number of neutrophilic granulocytes in peripheral blood almost to their complete disappearance. In the smear (when conducting an analysis), very few cells are presented mainly lymphocytes. Sometimes monocytosis, single reticular (process) cells and plasmocides are observed in peripheral blood. Anemia and thrombocytopenia are usually not observed, except in very difficult cases.
At leaving the state of agranulocytosis, a leukemoid reaction is often developing with the number of leukocytes of 30 g / l and above in peripheral blood, with the appearance of blast cells, promoelocytes, etc.
Such a picture is usually short-lived, it can be observed literally a couple of hours. Then, as the patient recovers, the blood indicators are normalized. The duration of immune agranulocytosis in most cases is one and a half - two weeks, sometimes more.
 Myelotoxic Agranulocytosis Most often arises as a manifestation of cytostatic disease and is characterized by the cessation of products of neutrophilic granulocytes due to the generation at the level of the predecessor cell of myelopoes or stem cell. In this case, not only the number of granulocytes, but also lymphocytes, platelets and red blood cells.
Myelotoxic Agranulocytosis Most often arises as a manifestation of cytostatic disease and is characterized by the cessation of products of neutrophilic granulocytes due to the generation at the level of the predecessor cell of myelopoes or stem cell. In this case, not only the number of granulocytes, but also lymphocytes, platelets and red blood cells.
The cause of the development of myelotoxic agranulocytosis can be drugs, metastatic tumor bone marrow lesions, leukemia, etc.
Patients even before the appearance of signs of the disease decreases the number of leukocytes, platelets and reticulocytes. Lakeing can develop - up to 0.5-0.1g / l. The number of neutrophilic granulocytes in peripheral blood sharply decreases almost to their complete disappearance.
Against the background of pronounced changes in the peripheral blood and in the bone marrow, angina appears, stomatitis, sometimes the bleeding of the gums, nasal bleeding, hemorrhage under the skin. In other cases, only the mucous membranes of the mouth and larynx are affected.
The reason for the lesion of the mucous membranes in myelotoxic agranulocytosis is to weaken the protective forces of the body, and therefore the actions of pathogenic microorganisms are activated. In addition, cytostatic (antitumor) drugs affect all proliferating cells, including mucous digestive channels. These changes can last from one or two weeks before the month and longer.
Before leaving the state of agranulocytosis in the bone marrow, a large number of myelocytes and blasts appear. Metamielocytes, myelocytes, monocytes and plasmocides are found in the perfectoric blood.
Forecast of agranulocytosis under aseptic (sterile) conditions, the use of antibiotic therapy, and in cases of immune agranulocytosis - and steroid therapy in most cases - favorable.