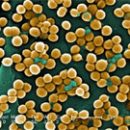
Endometritis is inflammation of the inner mucous membrane. Various microorganisms and their combinations are capable of calling it. Penetrating into the uterine cavity, pathogenic microorganisms are introduced into its mucous membrane, and an acute inflammatory response is developing.
Content
Matter women reliably protected from infection in it. Barriers on the path of infection stand and an acidic medium of vaginal secret, and the alkaline reaction of the cervical mucus. In addition, the cyclic update of the mucous membrane of the uterine cavity during the menstrual cycle contributes to the purification of the uterus from pathogenic microorganisms. The mucous membrane of the uterine of a healthy woman is less accessible to the penetration of infection in it than other organs of the sexual system. However, when weakening protection, or reducing general immunity, pathogenic microorganisms can still penetrate the uteros and cause it inflammation.
Causes of endometritis
Endometritis – This is inflammation of the inner mucosa layer of the uterus (endometrial). Various microorganisms and combinations are capable of calling this inflammation. Non-specific uterine inflammations are more often, but there are also specific, for example, with gonorly, tuberculosis and chlamydial infection.
Penetration of pathogens of microorganisms in the uterus can occur during menstruation from the vagina. During the period of menstruation, the cervical cervical channel is opened for the release of menstrual blood and microbes from the surface of the vulva and easily fall into the uterine cavity. This can be promoted by sexual intercourse and drew during menstruation. Sometimes infection can be listed in the uterus in the abortion, medical manipulations, in childbirth or in the postpartum period, if the rules of disinfection of tools, surrounding space or staff hands are violated. But more often the emergence of endometritis after surgery is observed in women having hidden genital infections.
Manifestations of endometritis
 Penetrating into the uterine cavity, pathogenic microorganisms are introduced into its mucous membrane, and an acute inflammatory response is developing. The mucosa is thickened, swells, becomes red, an ulceration appears on its surface. From the uterus begins to stand out abundant purulent discharge. If the inflammatory process applies further to the muscular layer of the uterus and then (parameter), the uterus increases in size, becomes flabby and sharply painful.
Penetrating into the uterine cavity, pathogenic microorganisms are introduced into its mucous membrane, and an acute inflammatory response is developing. The mucosa is thickened, swells, becomes red, an ulceration appears on its surface. From the uterus begins to stand out abundant purulent discharge. If the inflammatory process applies further to the muscular layer of the uterus and then (parameter), the uterus increases in size, becomes flabby and sharply painful.
Worsen and general condition of women. Increases body temperature, ailment, weakness, chills appear. Start disturbing stupid pulling pain at the bottom of the belly, which are often given to the seats and hips. Damaged by inflammation, the mucosa of the uterus begins to turn back and is manifested by the advent of blood impurities in purulent discharge, and sometimes bleeding not related to monthly. Menstruation themselves become painful, abundant, their duration increases. In addition, it should be borne in mind that if a woman has an intrauterine spiral, her presence in the uterus can take the course of the disease. When endometritis, the spiral is always removed.
Sometimes, during menstruation, and pathogenic microorganisms are removed from it from it and then in rare cases, self-symptition from endometritis is possible. If for 2-3 menstrual cycles do not take any treatment, sharp manifestations are silent and endometrite goes into a chronic form. Then the manifestations of the disease become less bright, but constant. Often the only signs of chronic endometritis are the absence of pregnancy, miscarriage, disruption of menstrual function and minor drawing abdominal pain.
If you summarize, the main complaints of a woman with acute endometritis are: an increase in temperature, weakness, fatigue, the presence of mucous-purulent discharge, often with blood impurity, the appearance of intermented bleeding, lengthening, strengthening the periods themselves and the occurrence of constant stupid pain at the bottom of the abdomen or hips. If it is your anxiety – Urgently go to the doctor gynecologist.
Diagnosis of endometritis
Survey complex with suspicion of acute, endometritis does not differ from that with all inflammatory diseases of the genital organs of women. These are strokes and crops separated from the vagina and the cervical canal to identify pathogenic microorganisms and the study of their sensitivity to antibiotics. With a vaginal two-way study, the detection of a slightly enlarged, soft and painful uterine will speak in favor of endometritis. The recognition of the disease in the acute stage in combination with the presence of purulent discharge from the uterus and the disruption of the menstrual cycle, the polling of women (preceding the intervention in the uterus, setting the intrauterine spiral, chronic inflammation of the genital organs, etc.) does not represent difficulties. The diagnosis of chronic endometritis is more complicated and requires hysteroscopy (inspection of the uterine cavity through a special optical device - a hysteroscope) and diagnostic scraping followed by the study of the material obtained. These surveys are already produced in the hospital, and not in women's advice.
So, the examination is completed, the diagnosis is set – Endometritis. What treatment offers modern medicine?
Treatment of endometritis
The treatment of endometritis is complex and wearing a phased character.
As soon as the endometrite originated, that is, in the acute stage of the disease, antibacterial therapy with an obligatory study of the sensitivity of the dedicated microorganisms to antimicrobial drugs is appointed. In addition, drugs can be assigned to reduce pain and reduce temperature. Next, drugs are used to restore normal microflora vagina, physiotherapy, drugs that increase the immune defense of the body and vitamins.