Thrombocytopenia - a condition characterized by a decrease in the number of platelets below 150 x 109 / l. and increased bleeding. What kinds of thrombocytopenia? Read more about it in the article.
Content
Thrombocytopenia
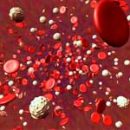
Platelet pathology is the cause of bleeding in almost 80% of cases. At the same time, thrombocytopenia is the most frequent manifestation. It is believed that normally the number of platelets should be within (150-400) × 109 / L. In normal physiological conditions, the number of blood platelets can fluctuate. It depends on the physical exertion, digestion, hormonal background, in women from the menstrual cycle - in the first days of menstruation it can decrease by 30-50%. Lifetime of platelets - 9-10 days. About 1/3 of blood plates deposited in a normal spleen. In cases where the number of platelets is less than 150 × 109 / l, the thrombocytopenia should be aspage. The frequency of this phenomenon is large enough - from 10 to 130 new cases per 1 million people.
Distinguish acute and chronic thrombocytopenia. The latter is diagnosed when it exceeds it 6 months. In persons with platelet levels above 50×109 / l extremely rarely bleeding. In this regard, many believe that in order to ensure a full hemostasis, there are enough platelets in the range of 30×109 / l, 15 and even 10×109 / l full platelet can provide effective hemostasis. It is probably why the thrombocytopenia is most often found in medical practice only as a laboratory phenomenon, causing surprise of doctors, because in no way manifests itself clinically. At the same time, a decrease in platelets is below 100×109 / l should attract serious attention to the doctor, since this symptom of thrombocytopenia may accompany a serious pathology. In this regard, the cause of each case of thrombocytopenia must be found out.
Hemorrhagic thrombocytopenia
Hemorrhagic thrombocytopenia was one of the first identified human hemorrhagic diseases. Distinguish several types of thrombocytopenia. Very often they are secondary, being a symptom of some disease. However, thrombocytopenia syndrome can often be independent, and its pathogenesis is different. Thrombocytopenia may be a consequence of the inferiority of platelet production, their increased destruction due to immune and non-immune mechanisms, as well as the redistribution in the body from the blood into individual bodies, more often a spleen, or their cluster in thrombotic masses with a massive intravascular blood coagulation. Frequent cases of combination of these reasons.
 However, the lack of clear criteria to confirm a certain
However, the lack of clear criteria to confirm a certain
The pathogenetic mechanism makes it use for practical
the doctor is not very desirable, since most doctors are trying
identify a specific nosological form, and then already
comprehend its etiology and pathogenesis. In this regard, it seems to us
It is advisable to immediately inform practical doctors information
Regarding the possibility of thrombocytopenia as a separate
secondary syndrome with some other disease.
First of all, the disease should be excluded,
able to cause coagulopathy consumption. These include all
infectious diseases in T.C. HIV infection; Neoplastic processes
any localization, especially the tumors of the liver, gastrointestinal tract, leukemia, etc.;
systemic autoimmune diseases primarily well as well as
Obstetric pathology due to a premature detachment of the placenta,
intrauterine fetal death, emboline by oily waters; Massive
Tissue damage as a result of injuries. Diseases such as
Drug disease, Auglobulinemia, lymphoproliferative
Diseases, inherited and acquired myelodysplasias also often
accompanied by thrombocytopenia.
Pathological deserves special attention
States accompanied by an increase in spleen. Most often that
Observed with portal hypertension of any genesis (liver cirrhosis,
Other disorders of the outflow on a muster vein), accumulation diseases
(Thezaurismos): Nimanne-Peak's disease, Hend-Shuller-Chrischena, Goshe,
Gemochromatosis and other., as well as with many of the states listed above
- infections, diffuse diseases of connective tissue and blood disease.
The occasionally splenomegaly is noted with a stagnant cardiac
Insufficiency. As mentioned earlier, in a normal spleen
Focus from 1/3 to 1/4 of all platelets. Therefore
Any increase in the spleen leads to an increase in the delay in it
platelets, which causes the thrombocytopenia phenomenon. At all
listed states will be more fair to assume
Possible presence of several pathogenetic mechanisms. An exception
or confirmation of many of the listed diseases often requires
big differential diagnostic work.
Secondary thrombocytopenia are due
Impact on the organism of radial energy, being a symptom of radiation
diseases, various toxic substances, in t.C. salts of heavy metals,
alcohol and other., Entering the symptom complex of pancytopenia. Likely such
The mechanism of thrombocytopenia in patients with uremia. It is possible that violation
The regulation of hemopower with vitamins and hormones has certain
Features for thrombocytopower, however thrombocytopenia
pernicious anemia should be considered only as a symptom,
Sometimes the main thing.
Primary thrombocytopenia, t.E. Those diseases,
Clinical manifestations of which are fully related to thrombocytopenia and
in which other pathology is not observed, also have different
Pathogenetic mechanisms, but these diseases deserve special
descriptions.
Thrombotic thrombocytopenic purpura (TTP) (Moshkovitz disease)
Thrombotic thrombocytopenic purpura (TTP) (Moshkovitz disease) was
First described by the author at a 16-year-old girl in 1924. The disease had
Acute start and manifested by fever, impaired kidney function and CNS,
Candular deficiency phenomena with severe thrombocytopenia. On the
An autopsy revealed a lot of blood clots in capillaries and small arteriols,
Almost entirely consisting of platelets and a small fibrin
Component. For the disease, a combination of pronounced
plateitopenia with intravascular hemolysis (with many
fragmented erythrocytes) and neurological manifestations - from
unwitting disruption of consciousness, motor and sensitive functions
Sailor and coma. These clinical manifestations in 70-90% of cases are
one-time, and only 10-30% of patients they recur at
Pregnancy, various infections, chemotherapy. In individual patients
They can recur through regular intervals. This allows
assume that TTP syndrome is heterogeneous and combines several
various diseases. Practical measures: Plasma Plasma Replacement
Patient on poor platelets Freshly frozen plasma of healthy
allow today to save up to 90% of patients recently doomed on
death.
Hemolytic-uremic syndrome
Hemolytic-uremic syndrome many
considered as a variety of TTP. However, the absence of pathology
nervous system, persistent arterial hypertension and pronounced renal
Pathology with progressive renal failure as well
The possibility of inheritance is forced to consider it
Self. Thrombocytopenia is pronounced, accompanied by
intravascular hemolysis - direct consequence of thrombotic occlusion
Vessels.
Drug thrombony persecution. Described pretty
Many cases of thrombocytopencies that follow therapeutic measures.
Initially, attention paid only on cases of thrombocytopenia,
accompanying treatment with radioactive drugs. Medicinal
Preparations can cause thrombocytopenia in various ways. Cytostatics
Caught to catch a thrombocytopoese in bone marrow. Hinidin,
Sulfonamides, Salicylates, Dipyridamol, Gold preparations, Cefalotin,
Timetoprix, A-Methyldop and others may include immune mechanisms.
They provoke thrombocytopenia, settled on platelets and stimulating
Education of antibodies to this complex. Other medicines form
complexes with plasma protein, which is then connected to
platelet membrane and leads to the development of antibodies to this
formation. Third cause the destruction of platelets themselves and thereby
contribute to the formation of antibodies directly to the last.
Recently, great attention is attracted
thrombocytopenia caused by heparin, or as some
Researchers, thrombocytopenia associated with heparinotherapy.
Almost 10% of patients receiving intravenously heparin, moderately reduced
The amount of platelets, which usually occurs within 1-2 days
After administration, the level of reduction rarely is less than 100 x 10nine/ L. Today it is already known that heparins are able to cause thrombocytopenia of two types.
The first type described above is due to direct
interaction of heparin with platelets. Its connection with the surface
platelets depends on the molecular weight of heparins, their sulfatization
and the degree of activation of platelet caused by these interaction.
Noted that the degree of thrombocytopenia decreases in parallel with
Reducing the molecular weight of the introduced heparin. Heparinniducan
Thrombocytopenia of the 1st type arises quickly after its introduction, sometimes
After a few hours, due to the change in platelet membranes,
which provide aggregation of platelets. This type of thrombocytopeny
quickly passes and danger for the patient does not represent.
Heparinniduced, or associated,
The thrombocytopenia of the 2nd type occurs between the 4-20th day after the introduction
Heparin with a maximum of severity on the 10th day in patients who received
Heparinotherapy for the first time. When re-introducing heparin, it can
Arrive in the first days after the introduction of the drug. This
Thrombocytopenia is due to immune mechanisms provoked
heparins responsible for the production of specific antibodies to
Thrombocyt. These antibodies are detected by almost 7.5% of patients,
receiving an unficing heparin produced from products,
obtained from pigs, and only in 2.5% of those who received
Low molecular weight heparins.
The mechanism of this thrombocytope differs from other
immune thrombocytopenia in that in this case the antibodies are not
Strengthening the phagocytosis of platelets by the system of macrophages, and stimulate
intravascular aggregation of thrombocyte. From other immune
Thrombocytopenia it also differs in that it is practically
There are no hemorrhagic complications, despite the fact that it
develops against the background of anticoagulant therapy. This thrombocytopenia is
The essence reflects the consumption of platelets in the formation of microtrombov,
which can increase to large sizes, determining
Thrombotic phenomena. The latter are dangerous and in cases where
Heparinotherapy does not stop, may be the cause of death
in 20-30% of cases.
Idiopathic thrombocytopenic purple
 Almost in 95% of cases based on thrombocytopenia lies idiopathic
Almost in 95% of cases based on thrombocytopenia lies idiopathic
Thrombocytopenic purpura (ITP). It is assumed and diagnosed,
when platelet reduction is not directly connected with any
cause or condition capable of calling this reduction. Annually
10-125 cases of idiopathic
thrombocytopenic purpura for every million people. Idiopathic
Thrombocytopenic purple is considered
acute if less than 6 months lasts, a longer existence
should be regarded as chronic idiopathic
Thrombocytopenic purple. Acute form idiopathic
Thrombocytopenic purpura more often
occurs in children and ends with complete recovery in 75%
Sicklaby. Adults more often suffer from chronic idiopathic version
thrombocytopenic purpura, while
Up to 5% of them die from bleeding, mainly from hemorrhage
in the brain. Analysis of a large number of patients with thrombocytopenia, which
Passed a full-fledged examination, including bone marrow research,
showed that the causes of thrombocytopenia other than idiopathic
Thrombocytopenic purpura, were only 4%
Examined. However, due to the fact that specific criteria for
diagnostics idiopathic
Thrombocytopenic purpura today is absent, its diagnosis
Based only at the exception of other causes of thrombocytopenia. At
this to properly determine the nature of the disease equally
Anamnesis data, physical characteristics of the patient, as well as important
Clinical picture and laboratory and instrumental results
Research. History can help first of all when finding out
Inherited pathology. In the presence of anomalies of development near the nearest
Relatives of the surveyed can be suspected and reveal inherited
Thrombocytopenia.
Inherited and congenital thrombocytopenia. At
the absence of a radiy (radial) bone to think about inherited
pathology - tar-syndrome (thrombocytopathy in the absence of radial
bones), which is also characterized by a defect release dense
platelet and thrombocytopathy. Thrombocytopenia combined with
Defect for hair pigmentation, leather, retina, obliges thinking about
In the patient inherited pathology - Chediak Higashi syndrome, which
It is also characterized by a defect release of platelet granules and, as
Corollary, thrombocytopathy. The presence of eczema and tendency to infectious
Diseases will always assume inherited pathology -
Syndrome Viscott-Aldrich, also with a defect release of dense granules
platelet and thrombocytopathy due to a platelet aggregation defect
Adrenaline. The presence in the blood smear of giant platelets gives
reason to assume both inherited Maya-Hegglin syndrome and
Bernard Sulie. Their difference is that when syndrome
Maya-Hegglin can be found in the blood abnormal granulocytes with large
Inclusions, and during the disease Bernara Sulie, a defect is detected
LB glycoprotein, which determines platelet adhesion to factor
Willebranda. It is possible that some thrombocytopenia of newborns
Causes inherited thrombooetin deficiency.