Hemolytic anemia is an extensive group of diseases differing from the reasons for the emergence of development mechanisms, the main symptoms and treatment methods. The main feature of hemolytic anemia is the increased collapse of the erythrocytes and shortening the duration of their life.
Content
The concept of hemolytic anemia
Hemolytic anemia is a group of diseases, the main sign of which is the increased decay of the red blood cells. In physiological conditions, the life expectancy of erythrocytes is 100-120 days. Olderocytes are destroyed in sinus spleen, as well as in the bone marrow.
The pigment of bilirubin, resulting as a result of the physiological decline of erythrocytes, circulates in the blood in the form of a free (indirect) bilirubin, which is transported to the hepatic cell, where, with the participation of enzymes penetrates from hepatic cells in bile moves and stands out with bile in the intestine.
In hemolytic anemia due to the strengthened destruction of red blood cells, their life expectancy is shortened to 12-14 days. Accelerated hemolysis (erythrocyte destruction) can be mainly intracellular or intravascular. The intracellular decay of the erythrocytes occurs in the cells of the reticulogisticism system, mainly in the spleen, and is accompanied by an increase in the indirect bilirubin, which is allocated with urine and feces. In case of intravascular hemolysis, hemoglobin enters in an increased amount of blood plasma and is released with urine unchanged or in the form of hemosiderin, which can be deposited in the internal organs and cause hemosiderosis.
Options for hemolytic anemia
Hemolytic anemia for flow can be acute or chronic. All hemolytic anemia is divided into congenital (hereditary) and acquired.
Hereditary hemolytic anemias are a consequence of various genetic defects in red blood cells, which become functionally defective and unstable.
Acquired hemolytic anemia are associated with the impact of various factors contributing to the destruction of red blood cells (antibody formation, hemolytic poisons, mechanical impacts, etc.).
The group of hereditary hemolytic anemia includes:
- Hemolytic anemia associated with violation of the erythrocyte membrane (microspherocytosis, ovalcitosis, stomatocytosis)
- Hemolytic anemia associated with violation of enzyme activity in red blood cells
- Hemolytic anemia associated with violation of the structure or synthesis of globin chains (thalassemia, sickle cell anemia, anomalous hemoglobin carriage)
The group of acquired hemolytic anemia includes:
- Hemolytic anemia related to the effects of antibodies (isoimmune, autoimmune)
- Hemolytic anemia associated with the change in the structure of the erythrocyte membrane due to osmotic mutation
- Hemolytic anemia associated with mechanical damage to the erythrocyte shell (heart valves prostheses, marching hemoglobinuria)
- Hemolytic anemia associated with chemical damage to red blood cells (hemolytic poisons, lead, heavy metals, organic acids)
- Hemolytic anemia related to the lack of vitamin E
- Hemolytic anemia related to the effects of parasites (malaria)
Hereditary hemolytic anemia is divided depending on the location of the genetic defect in the erythrocyte (membrane, enzymes, the structure of the globin). The most common hereditary disease of the first group is microspherocytosis (Minkowski-Shoffhara disease). It is much less likely to occur ovalocytosis and stomatocytosis. Most of the diseases of this group can be recognized by the form of erythrocytes.
Another group of hereditary anemia is due to the deficit in the erythrocytes of various enzymes. Hemolysis (decay) is often provoked by the reception of some drugs. The third group of hereditary hemolytic anemia is associated with impaired hemoglobin formation, which is reflected in the red blood cells and their resistance to different impacts. A typical representative of this group is a sickle cell and target-cell anemia (Thalassemia).
Most of the hemolytic anemia acquired are associated with the impact on antibody red blood cells. A special form among acquired hemolytic anemia is a Markiafa-Mikekel disease (Permnetable intravascular hemolysis).
The main symptoms and treatment of hemolytic anemia
 The main symptoms of the disease depends on the severity of hemolysis. In most cases, the first signs are detected in youthful or mature age. In children, the disease is usually detected by examining the diseases of their relatives. Complaints outside the exacerbation of the disease may be absent.
The main symptoms of the disease depends on the severity of hemolysis. In most cases, the first signs are detected in youthful or mature age. In children, the disease is usually detected by examining the diseases of their relatives. Complaints outside the exacerbation of the disease may be absent.
During the period of exacerbation, weakness, dizziness, temperature rise. One of the main symptoms is the jaundice, which for a long time can remain the only sign of the disease. The severity of the jaundice depends on the one hand, from the intensity of hemolysis, and on the other - on the ability of the liver to binding free bilirubin. In the urine bilirubin is not detected, since free bilirubin does not pass through the kidneys. Cal intensively painted in a dark brown.
The cardinal symptom of hereditary microspherocytosis is the increase in the spleen, which protrudes from under the rib arc by 2-3 cm. With long-term hemolysis, there is a significant increase in the spleen, in connection with which the patients complain about the severity in the left hypochondrium. The liver is usually normal sizes, sometimes its increase is found. The severity of anemic syndrome is different. Often there is a moderate reduction in hemoglobin. Some patients have no anemia in general. The most sharp decrease in the number of red blood cells and hemoglobin is observed during the period of hemolytic crises.
In persons of middle and old age, there are sometimes poorly treatable trophic shin ulcers associated with the collapse of red blood cells in small capillaries of limbs. The course of the disease is characterized by so-called hemolytic crises, manifested by a sharp increase in symptoms against the background of continuous current hemolysis. Hemolytic crises usually arise after infections, when heocoled, in women - in connection with pregnancy.
The only method of treating patients with hereditary microspherocytosis is the removal of a spleen, which turns out to be effective in 100% of cases. After the removal of the spleen in patients occurs practical cure, despite the fact that red blood cells retain their pathological properties (microspherocytosis, decrease in osmotic resistance). The removal of the spleen is shown in frequent hemolytic crises, harsh anemia, spleen infarcts, renal colic.
As a preoperative preparation of patients showing the transfusion of the erythrocyte mass.
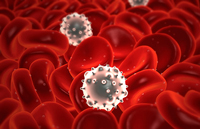
Acquired autoimmune hemolytic anemia is associated with an increase in the organism of the patient antibodies to its own red blood cells, which glued and decay in the spleen. Most common in chronic lympholoicosis, lymphoganuzomatosis, acute leukemia, systemic red lupus, rheumatoid arthritis, chronic hepatitis and liver cirrhors.
For currents allocate acute and chronic autoimmune hemolytic anemia. With sharp forms in patients suddenly there is a sharp weakness, heartbeat, shortness of breath, fever, jaundice. In chronic forms, the disease develops gradually. An objectively revealed an increase in spleen, less often - liver.
The means of choice in the treatment of autoimmune hemolytic anemia are glucocorticoid hormones (prednisone), which almost always stop or reduce hemolysis. A prerequisite is sufficient dosage and duration.
In the acute phase it requires 60-80 mg / day (at the rate of 1 mg / kg of mass) of prednisolone. As the state of the dose of prednisolone is gradually reduced to supporting. Supporting dose - 5-10 mg / day. Treatment is carried out for 2-3 months before all signs of hemolysis disappears.