How does asthma treatment occurs in pregnant women? How to control the disease during pregnancy? How to avoid exacerbations of the disease? Answers to these questions you will find in the article.
Content
Treatment of asthma and pregnancy
First of all, the treatment of a pregnant woman must appoint a doctor. Close contact with a specialist - a necessary condition for successful treatment: only so you can achieve maximum effect at minimal risk. All medicines are applied according to the principle: «Only if the expected benefits exceeds the possible risk for mother and fetus». Particularly strict requirements are presented with respect to 1 trimester of pregnancy as the most vulnerable in terms of any impacts.
In the treatment of asthma, preference is given to the topical (active locally) inhalation drugs, since the concentration of the drug in the blood is minimal, and the local effect in the target zone, in bronchi, maximum. It is recommended to use inhalers that do not contain freon. Dosage aerosol inhalers should be applied with spacer to reduce side effects risk (Read more...). A prerequisite for successful treatment is the correctness of inhalation (inhalation technique). Master the necessary skills will help the pulmonologist or instructor in the classroom in Asthma school.
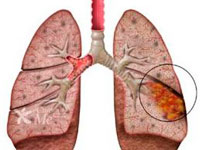
It has been established that bronchial asthma regardless of gravity is a chronic inflammatory disease. It is the constant presence of this special chronic inflammation in bronchi is the reason for the emergence of symptoms. If only to treat the symptoms (eliminate the spasm of bronchi), but it does not fight for their reason, the disease will progress. Therefore, the treatment of bronchial asthma is made up of basic therapy (drugs for disease control) aimed at controlling inflammation, and drugs to facilitate the symptoms and treatment of exacerbations. The volume of basic therapy determines the doctor depending on the severity of the flow of asthma. Adequate basic therapy significantly reduces the risk of exacerbations and allows you to minimize the need for preparations to facilitate symptoms.
On the safety of the use of drugs
In our time, medicine has become evidence, t.E. Each recommendation, each concept, each drug, before you get approval and permission to use, must be thoroughly verified by certain scientific rules. A fully safe drug is considered only when its safety is verified and proven during the so-called double-blind randomized placebo-controlled large-scale clinical studies, in which the effects of this drug are compared both with known drugs and absence of interference. In this case, the study is built so that the beliefs or prejudices of the doctor or patient could not affect final conclusions. But the conduct of such research in pregnant women is almost impossible for ethical considerations. Safety has to be judged according to the data obtained on animals, and according to the results of long-term observations of the outcomes of pregnancies in people. Therefore, no preparation used for bronchial asthma has not been assigned the highest level of security - Category A («Placebo Safety», testifying that the reception of the drug affects the safety indicators no more than if the drug did not apply at all).
All drugs have been assigned a certain category of safety application during pregnancy. Unfortunately, this is usually not indicated in the instructions for the drug. So, the drugs categories and at the moment there is no. The following security category, category B, is assigned to drugs that were safe in animal studies, or, even if animal tests revealed a side effect, managed to confirm that for people the drug is safe even in vulnerable pregnancy periods. If the possible use of applications exceeds the risk of complications, or safety data is simply not enough, the drug receives a category with. Category D includes drugs having a proven side effect, but at the same time possible benefits may allow them to use, despite the risk. Category X - drugs with teratogenic action, the risk of their use exceeds possible benefits, and during pregnancy they do not apply.
Preparations that will help facilitate the state
 A pregnant woman should not tolerate or survive the attacks of suffocation so that the lack of oxygen in the blood did not damage the development of the future child. So, a drug is needed to relieve symptoms.
A pregnant woman should not tolerate or survive the attacks of suffocation so that the lack of oxygen in the blood did not damage the development of the future child. So, a drug is needed to relieve symptoms.
Preparations of choice are inhalation beta2 agonists with a rapid start of action. Prefer elective drugs, selectively affecting bronchi with minimal effect on the cardiovascular system. «Gold standard» In Russia, Salbutamol (Salbutamol, Ventoline, and others.), in the world - terbutalin (Brikanil Turbukhaler). Terbutalin is considered optimal (Category B), but in our country it is much more expensive and less available than Salbutamola preparations. The nebulizer form of terbutaline in our country is not registered, so if necessary, only Salbutamol applies in nebulizer therapy.
The use of these drugs during pregnancy requires caution and medical observation. The limitations are primarily related to the fact that the injection forms of beta2 agonists are able to relax the muscles of the uterus, and therefore, in the threat of miscarriage in 1 and 2 trimester of pregnancy, premature detachment of placenta, bleeding and toxicosis in 3 trimester, there is a possibility of gaining bleeding. In the inhalation and in the recommended doses, the impact on the muscles of the uterus is very small, but this theoretical opportunity is taken into account. The uncontrolled use of bronchodilians at the end of pregnancy can extend the duration of labor.
The use of fhenoterol (Berotek) and Berodala (combination of fenoterol with cholinolitic) in the first trimester of pregnancy avoid, but admit if the expected benefit exceeds the possible risk. The studies did not reveal a negative impact on pregnancy, but the available data is not enough to remove restrictions. For inhalation cholinolithics (IPratropium - Atrovant), negative impact on the development of the fetus (Category B), but this drug is usually not used for the treatment of asthma (only in combination), since it develops more slowly.
In pregnancy, it is absolutely contraindicated by the use of any ephedrine preparations (theofedrine, powders for Kogan and T.D.) because the ephedrine causes the narrowing of the vassels of the uterus and exacerbates the hypocia of the fetus. The use of adrenaline on the exacerbations of bronchial asthma is not recommended (it is desirable to use terbutalin in an injection form).
The frequency of the use of bronchodilists is an important indicator of the control of asthma. With an increase in the need for their application, contact the pulmonologist to enhance the planned (basic) therapy for disease control. Treatment only with drugs to facilitate symptoms is permissible only in the easiest cases with rare non-heavy symptoms and with rare non-heavy exacerbations. As follows from their name, these drugs are able to remove the symptoms already emerged, but do not have anti-inflammatory activity and do not affect the control of the disease.
What is planned therapy
The planned (basic) therapy for the control of the disease must necessarily correspond to the severity of the disease, which is a prerequisite for reducing the need for preparations, expanding bronchi, and warnings of exacerbations. If the severity of asthma requires mandatory basis therapy, and the patient only removes the symptoms, asthma becomes uncontrollable, dangerous for the mother and harm the fetus. The purpose of the planned therapy necessary to control asthma, prevents attacks and exacerbations that cause hypocia of the fetus,.E. promotes not only the normal course of pregnancy, but also the normal development of the child.
Surrounded by a pregnant woman with bronchial asthma will always be found «kindness» (sometimes even physicians or - more often - former doctors), trying to infect a woman with fear of treatment and drugs applied. Always remember: you breathe for two, and unreasonable fears are not allowed. Do not listen to the highly different and small «Neighbor Babu Manya». Focus only on the information obtained from a qualified specialist.
Control of the disease
Cromons (Intal, Tayly) apply only with a mild persistent asthma. If the drug is appointed for the first time during pregnancy, sodium crumglikat (Intal) is used. If the patient before pregnancy received an unoccupatic (tillage) with a good effect, the therapy continues. But if cromons do not provide adequate disease control, inhaled hormonal drugs must be appointed.
Inhalation hormones - the basis of the basic therapy of persistent asthma in all cases, except the easiest. The appointment of them during pregnancy has its own characteristics. If the drug should be appointed for the first time, it is preferred by budesonide (bulvikort): Analysis of 2014 pregnancies, conducted in 2000, did not reveal the increase in risk for the fetus (the drug was submitted to category B). Becmenetazone, more affordable in our country can also be appointed. If the pregnancy of asthma was successfully monitored by another inhalation hormonal drug, it is possible to continue this therapy. With the ineffectiveness of medium doses, the doctor can add theophylline preparations (with great caution) or Salmetterol. For the use of theophylline (both euphilline and prolonged drugs in tablets, such as the theorec) during pregnancy, are greater caution, especially in the 3 trimester, when the movement rate of theophylline from the body decreases: this drug freely penetrates the placenta and can cause tachycardia and violations Rhythm from the fetus and newborn.
Leukotriene antagonists can be used with caution and only in strict indications. Security class - in.
Preparations are prescribed only individually, especially since this rule should be observed during pregnancy. The volume of treatment required at a given severity of the bronchial asthma determines the doctor who is observing the patient, while focusing, besides the clinic of the disease, on the picoflorometry data.
ASTME Action Plan
Bronchial asthma is one of those diseases that require a patient ability to control their condition. Just as a tonometer is needed in hypertension, and in the treatment of diabetes mellitus - a glucometer, for self-controls during asthma, a portable and easy-to-use device is developed, which is called picofloumetr.
The recorded indicator is the peak rate of exhalation, abbreviated PSV - allows at home to monitor the disease.
Register the testimony should be 2 times a day, in the morning and in the evening, before the use of bronchoditics, as well as when symptoms appear. Data is recorded in the form of a graph, as it gives more information: not only specific numbers, but also the form of the resulting graph. One of the alarming symptoms are «Morning failures»: Periodically registering low rates in the morning hours. «Morning failures» - Sign of incomplete control of asthma and early symptom of impassive exacerbation.
Tangible changes in well-being can still be absent, and on time taken to avoid the development of exacerbation. Self-controlling with a picoflorometer is a prerequisite for compiling ASTME Action Plan: Detailed recommendations of the doctor in which basic therapy and necessary actions are scheduled for changes.
How to treat exacerbations
The most important thing is to try exacerbations to prevent. Measures to limit contact with allergens and properly selected planned therapy significantly reduce this risk. But the exacerbations are still happening, and the most frequent cause is ORVI.
The aggravation of bronchial asthma Along with the danger to the mother, is a serious threat to the fetus due to the development of hypoxia, so the delay in treatment is unacceptable. Treatment of exacerbations requires the use of a nebulizer, the drug of choice in our country is Salbutamol. The effect of treatment is estimated not only clinically, but also with the help of a picoflorometer: if after the treatment, the figures did not reach the level of 70% of the normal (or the best for a given patient), urgent hospitalization is necessary. If necessary, inhalation cholinolics (atrownt) can be connected to nebulizer therapy, with insufficient effect, Eufillin intravenously is appointed. Oxygen therapy is used to combat fetal hypoxy.
With heavy exacerbations of bronchial asthma requires the use of systemic hormonal drugs, including tableted hormones with a short course; At the same time, the preparations of trimcinolone (PolcorTolon) are avoided due to the risk of influence on the muscular system of mothers and the fetus, as well as dexamethasone and betamethazone, and preference is given to prednisolone or methylprednisolone drugs. Harm that inflicts hypoxia to the child is multiple times higher than possible side effects.
As already mentioned, in pregnancy, the use of any ephedrine drugs is absolutely contraindicated, since it aggravates the hypocia of the fetus. The use of adrenaline on the exacerbations of bronchial asthma is not recommended.
More about medication therapy
To the appointment of any drugs during pregnancy should be treated with caution, including painkillers and vitamins. Caution when taking non-steroidal analgesics (aspirin, analgin and t.D.) It is necessary for all patients with bronchial asthma, and with aspirin asthma requires a complete and absolute elimination of all drugs of this group.
The intolerance of any medicines is not uncommon with bronchial asthma. You will be more security if you always have a patient with an allergic disease filled with an allergist, where drugs previously caused an allergic reaction or contraindicated during asthma (for example, beta-blockers), as well as related drugs that may be Cause crosst allergies. Before applying any medication, you need to familiarize yourself with its composition and instructions for use, and all the questions that have arisen with the doctor.
As already mentioned, during pregnancy, it is absolutely contraindicated by the use of any ephedrine preparations (including theofedry), since it causes the narrowing of the vassels of the uterus and exacerbates the hypoxia of the fetus. Application of adrenaline about the exacerbations of bronchial asthma is not recommended (if necessary, thermal injecting is used).
Neither about asthma, nor with allergies during pregnancy, the deposited forms of system hormones of long-term action - Kenalog, Diprospan.
Sometimes special measures are required to combat the heartburn of pregnant women, t.To. It can adversely affect asthma, especially at night hours. It is very important to the appointment of a diet with the exception of caffeine, chocolate and other provoking heartbuzz products, in some cases it is required to prescribe medication.
In the presence of concomitant diseases that require planned therapy (for example, hypertension), it is necessary to contact a specialist of the appropriate profile to correct therapy with the planned pregnancy.
From expectorant drugs are contraindicated with the drugs of iodine or iodine-containing substances (for example, potassium iodide), since they can affect the fetal thyroid function.
Allergic antihistamines are not used for the treatment of bronchial asthma in adults, but the need for them may be associated with the presence of other allergic diseases, for example, with a concomitant allergic rhine. They have significant restrictions on use during pregnancy, especially in the first trimester. Only a limited amount of drugs under the strict control of the doctor, in small doses and in strict testimony (for example, diphenhydramine - DIMEDROL). Modern antihistamines are applied during pregnancy to the appointment of a doctor only in cases of extreme necessity, when the expected benefit exceeds the possible risk to the fetus (the experience of their use during pregnancy is not enough, in experimental studies on teratogenic action, category B): Cetirizin (Zirtek) , Loratadine (Claritin). Fexofenadine is currently attributed to the C category (information about its safety during pregnancy is currently missing) and usually not applied. It is allowed to use with special care of the Memomethazine (Primalana). It is unacceptable for the use of asthymizol and thermophodine (arrhythmogenic effect, identification of embryotoxic action on animals).