Hemolytic disease of newborns, erythroblastosis of the fetus (Erythroblasts - young forms of red blood cells), the disease manifested from the moment of birth or from the first hours of life of the child, most often in the incompatibility of the blood of the mother and the fetus in the rhesus factor.
Content
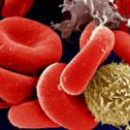
Erythrocytes of man (simply speaking, red blood balls) on their surface have various antigens. It is they who define a group or reserves-owner affiliation. A group of such antigens determines the blood-rescue factor, positive (RH +) in 85% of people on the planet and negative in the remaining 15% (RH-), all the horrors and fears related to the fact that the future mother has a negative reserves factor in It is often hypertrophy. With a competent attitude to their own health, it is quite possible to avoid many troubles.
Facts
The percentage ratio of reserves-positive and rezes-negative people in any country depends on the racial affiliation of the population and geographical features of the area. So, among the purebred blacks and the Chinese there are no rezes-negative people, if anyone is determined by negative rhesus, it means that there was a white man among the ancestors. It is also curious that the north the country or the country, the greater the rezes-negative inhabitants, and vice versa.
The basis of conflict
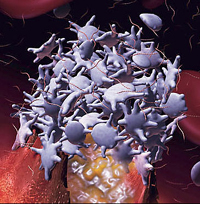
Rhow-factor in the fetus appears already in 7-8 weeks of pregnancy, that is, with a latency of menstruation for 3-4 weeks. If the future mommy rhesus is negative, and the daddy - rhesus-positive, is the likelihood that the child from his father will inherit a positive rhus. Protective forces of the maternal body recognize the fruit rezes as something alien and produce tie proteins (antibodies). They penetrate the placenta and destroy the red blood cells, causing hemolytic disease. The production of antibodies occurs after the direct contact of the blood of the mother and the fetus.
If both parents are negative, pregnancy always proceeds safely, since the child will also be a rezes-negative. Most often, with the normal course of the first pregnancy, the rhesus conflict does not occur. However, sometimes in childbirth, as well as detachment of the placenta, when conducting such manipulations during pregnancy, such as genetic amniocentesis (fence of oily water bubble) or cordocentsis (blood pressure from veins of umbilical cord), the blood of the fetus may occur in the mother's blood flow, The result of which antibodies are produced to rhesus.
If a woman has already had a childbirth or abortion, spontaneous miscarriages, an ectopic pregnancy on the period of more than 7-8 weeks, that is, the probability that the next pregnancy may have a rhesv conflict (the likelihood of such a conflict is not more than 10%).
Diagnostic methods
Hemolytic disease
There are methods of diagnosis that helps the doctor before delivery to navigate, what kind of rhesus in the fetus of the rezes-negative motley and whether the conflict occurs, and in the event of a hemolytic disease, it is evaluated to evaluate its severity.
 Titress (number) of antibodies to the blood rhesus Mom - an empty stomach of veins of moms take blood and look, whether there are antibodies in it to rhesus, and if there is, then in what quantity. If the serum antibodies are not detected or detected in small credits, they repeat the study in dynamics: 1 time every 4 weeks up to 20 weeks of pregnancy, then by testimony - 1 time in 2-4 weeks up to delivery.
Titress (number) of antibodies to the blood rhesus Mom - an empty stomach of veins of moms take blood and look, whether there are antibodies in it to rhesus, and if there is, then in what quantity. If the serum antibodies are not detected or detected in small credits, they repeat the study in dynamics: 1 time every 4 weeks up to 20 weeks of pregnancy, then by testimony - 1 time in 2-4 weeks up to delivery.
If the titer of antibodies are dubious or high, then amniocentesis is carried out - the fence of the oily water from the fruit bubble under the control of ultrasound. Determine the optical density of water, the titer of antibodies to the rhesus, as well as the fruit group. With a high optical density of the octal water, which indicates the decay of erythrocytes of the fetus, decide how to continue to maintain pregnancy.
Cordsenthesis - Blood Taking from Vienna Undergrades under the control of the ultrasound sensor. Determine the blood group and fruz factor, the titer of antibodies to the rhesus, the level of bilirubin, is there any anemia in the fetus (hemoglobin level). If after research it turns out that the fruit is rezes-negative, like mommy, then in the future dynamic observation there is no need. Of the modern diagnostic methods - the definition of RHD (one of the reserves-antigens, the main) fetus in the blood or in the mucus of the cervical channel of the mother. If the RHD of the fetus is not determined, it means that the froza is negative and in further observation there is no need.
A ultrasound examination also helps in the diagnosis: the thickening of the placenta, multi-way, as well as an increase in the size of the spleen and the liver of the fetus, the accumulation of fluid in its tummy can be manifestations of this disease. Methods such as amniocentesis and cordocentsis, sometimes lead to an increase in the titles of the blood of the mother's blood. Abroad, if, according to the results of these procedures, it turns out that the frozen-positive fruit is injected with an immunoglobulin antiresus (in a smaller dose than after childbirth)
If the mother is diagnosed with high antibody titers to Rhus
If the mother diagnoses high antibody titers to the rhesus, the high optical density of the octoral water, there are ultrasound signs of the hemolytic disease of the fetus, then treatment is carried out.
- Intravenously poured vitamins, glucose solution.
- Intravenously entered human immunoglobulins every 4 weeks before delivery. This helps to reduce the titer of antibodies to Rh.
- Purge Plasmapheres. The essence of the method is in the blood intake of the mother in the volume of 250-300 ml, then the shaped elements (red and white blood balls) are returned back to the vascular channel, and the elevated liquid part (plasma) of the blood is replaced by other healing solutions (albumin, reopolylukin, and T.D.). Thus, it is carried out as if the mechanical cleansing of the blood of a mother from antibodies to the reserves, which are contained in the plasma. This treatment method is applied from the second half of pregnancy.
- HemoSorption - removal of toxic substances from the blood using a special apparatus in which blood is passed through filters. In our case, the blood purification of the mother from antibodies to the rhesus is happening, then it returns back to the vascular channel.
- Intrauterine transfusion of rezes-negative single-log blood fruit from 18 weeks of pregnancy.
There are two blood transfusion methods.
- Blood under the control of ultrasound examination is introduced into the tummy of the fetus, from where it is absorbed into his bloodstream.
- In-insanity transfusion - is also carried out under the control of ultrasound examination: through the puncture of the front abdominal wall, the walls of the uterine with a long needle fall into the vein of the umbilicals and introduce a rhesus-negative blood, taking into account the blood group of the fetus.
Inserted rhesus-negative blood is not destroyed by the antibodies of the mother, in contrast to the own blood of the fetus.
Prevention of hemolytic disease
It is impossible to carry blood transfusion without taking into account the reserves-accessories of the donor and the patient. If the woman is rezes-negative, it can only be pouring a rhesus-negative blood if it is rhesus-positive - only rhesus-positive.
A woman with negative rezes need a reliable way of contraception. After all, any interruption of pregnancy can lead to the appearance of antibodies to the blood of the mother's blood.
After interrupting pregnancy for a period of more than 7-8 weeks, it is immediately necessary to introduce anti -usus immunoglobulin, containing antibodies to rhesus, which bind the fruit antigen and prevent the formation of their own antibodies to it.
If during pregnancy, the rezes-negative mommy was performed by amniocentesis or cordocentsis, after it is necessary to introduce antipers - immunoglobulin at a dose of 100 μg. In Russia, such prevention is not yet carried out.
After childbirth, a rezes-negative mammy is determined by the Rh. In the case of the birth of a rhesv-positive child, antveusus is introduced - immunoglobulin, if the mammy has not yet been sensitized (the titers of blood antibodies are not high). Immunoglobulin is introduced no later than 72 hours after delivery. Such prevention protects the fetus during subsequent pregnancy. After cesarean operations, the seventure or manual separation of the dose of the drug double.
Currently, in some countries, all women with rhesse-negative blood, with normal antibody titers to Rhus, in 28-34 weeks of pregnancy, anti -usus-immunoglobulin is administered, of course, if the Father Rus-positive.
Vice versa
There is a reverse situation - Mom Rus-positive, and daughter - Rh-negative. During such pregnancy, the conflict does not occur. However, in childbirth, the girl can be sensitized by the Mother Antigen. Because of this, the daughter from birth can be present antibodies to rhesus. And when it becomes mom, in the case of a rhesus-positive fetus, there may be a rhesus conflict pregnancy.
As we give birth
In the event of a rhesus conflict, hospitalization is recommended in 34-35 weeks of pregnancy for surveys and prepare for childbirth. Usually, labor is carried out naturally in 37-38 weeks of pregnancy, however, with severe manifestations of the hemolytic disease of the fetus - ahead of time, since lebid child is easier outside the womb than intrauterine. After birth, neonatologists are engaged in: carry out all research and treatment aimed at eliminating anemia, jaundice, edema. If necessary, the kid is carried out replaced blood transfusion and hemosorption.