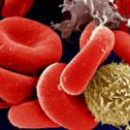
In the overwhelming majority of cases, the first pregnancy near the Rh-negative woman proceeds without complications. The rhesus factor is contained in blood cells, mainly red blood cells.
Content
Blood group and rhesus factor
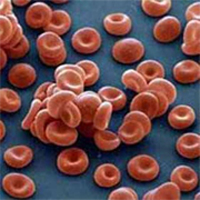
Every woman from a young age should know their blood group and a rhesus factor. According to statistics, approximately 15-20% of the female population have a rhesus-negative blood factor. The rhesus factor (or the reserves-antigen) is a protein that can be on the surface of red blood cells (blood cells that carry oxygen to the tissues). About 85% of people have a Rh factor and, accordingly, are rhesus-positive. The remaining 15%, who do not have it, - Rh-negative.
The threat of the rhesus conflict during pregnancy is due to a combination of two factors: (1) Woman Rus-negative, and the father of the future child - Rus-positive; (2)
The fetus inherits from the father of the gene responsible for positive rhesus, t.E.
Future baby Res-positive. In this case, in the body of the future
Mother may begin the formation of anti-episosis antibodies. IN
if both parents are reversely negative, the conflict threat is not
There is (the child will definitely be a rezes-negative). Same
Conflict's threats do not exist if a woman Res-positive
(Father's rhesia and child affiliation do not have any meanings). Besides, in
The case of a rhesus-negative mother and a rhesus-positive father has
A small probability that the fruit will inherit from both parents
genes responsible for negative rhesus and the rhesus conflict will not arise.
Resh antibodies
Connections of protein structures that are produced in the maternal
The body in response to the rhesus-positive erythrocytes in it
fetus (the immune system of the future mother perceives these erythrocytes as
alien). When detecting in the blood flow of the Mother's reserves antibodies Obster
Maintains diagnosis: Resh sensitization. This happens
artificial or spontaneous interruption of uterine or ectopic
Pregnancy. Rhose antibodies may also appear after the first birth,
If born baby Res is positive (during childbirth baby's blood
It falls into the bloodstream of the mother, causing the appropriate reaction).
Sensitization of the organism of a rhesse-negative woman is also possible at
transfusions of rhesv-incompatible blood (even if such transfusions
conducted in early childhood).
a pregnant woman begins with the moment of the formation of rezv antigens in
Erythrocytes of fruit. Because the antigens of the rhesus are contained in the blood
fetus from 7-8 weeks of pregnancy, then in some cases early
Sensitization of the body of the mother. However, in the overwhelming majority
cases of the first pregnancy at the Res-negative woman (with
the absence of the body's sensitization) flows without
Complications.
subsequent pregnancies, especially in case of interrupting the first
pregnancy, bleeding during the first pregnancy, with manual
Branch of the placenta, and also if the childbirth is carried out by caesarean sections
or accompanied by significant blood loss. This is explained by
With listed complications, the likelihood of a large
the number of rhesus-positive erythrocytes in maternal blood flow and how
Corollary - the formation of a large number of rhesus antibodies. Besides,
When first pregnancy, the immune system of the future mother is found with
reserves-positive erythrocytes of the fetus for the first time. Therefore, antibodies
It is not so much produced: about as much as you need for
the destruction of erythrocyte erythrocytes entering the blood. Besides,
These antibodies relate to class M immunoglobulins having large
Dimensions and poorly penetrating through the placenta to the fetus.
 But after childbirth in
But after childbirth inWomen's body remain «Memory cells», who are at the following
Pregnancies will be able to «organize» Fast and powerful antibody production
against rhesus. These will be already an antibody type -
Class G immunoglobulins that have smaller sizes than
Immunoglobulins M, and therefore, it is easier to penetrate the placenta and
are more aggressive. Therefore, the reaction of the female immune system
on the reserves-antigen of the fetus at the second and third pregnancy much
more quickly and tougher than with the first. Accordingly, higher and risk
Being fruit.
Medical literature, after the first pregnancy, immunization arises
10% of women. If a woman with rhesse-negative blood escaped
rezv-immunization after the first pregnancy, then the next
pregnancy rhesv-positive fruit The probability of immunization again
is 10%.
Future health
Moms Rezv-sensitization does not harm, but it can represent
Danger for the child. Finding into the bloodstream of the fetus, rhesus antibodies
Destroy its red blood cells, causing anemia (reduced hemoglobin),
intoxication, violation of the functions of vital organs and systems. That
The condition is called hemolytic disease (hemolysis - the destruction of red blood cells).
The collapse of the erythrocytes leads to damage to the kidneys and the brain of the fetus.
Since red blood cells are continuously destroyed, its liver and spleen
try to accelerate the production of new erythrocytes, while increasing
Sizes. In the end, they do not cope and they. It comes strong
Oxygen starvation, and a new round of heavy violations is launched in
Child's body. In the hardest cases, it ends it
intrauterine death at different times of pregnancy, in lighter
Rhow conflict manifests after the birth of jaundice or anemia
Newborn. Most often, hemolytic disease is developing rapidly
child after birth, which contributes to the admission of big
The number of antibodies in the blood of the baby when violating the integrity of the vessels
Placets.
Treatment of hemolytic disease
Complex, complex, sometimes baby requires replaced transfusion
blood. Doctors introduce him to the rezes-negative blood of his group and spend
Resuscitation events. This operation must be implemented in
36 hours after the child's appearance.
If it turns out that Woman Rus-Negative
The main thing in solving the problem of the reserves conflict is its prevention.
Determine the blood group and the Rh factor is preferably before pregnancy.
If it failed to do this before pregnancy, then in the women's
Consultation at the first turnout is determined by the definition of reserves.
If it turns out that a woman is negative, it takes it on
Special account. All pregnant women with rhesse-negative blood should
Examined regularly for reserves antibodies in blood serum. At
Antibody discovery must be applied to specialized
Medical centers for further observation.
IN
Arsenal leading obstetric clinics there is modern equipment,
allowing to follow the state of the fetus, diagnose the degree
gravity of hemolytic disease and, if necessary, carry out the main
Therapeutic event - intrauterine blood transfusion (under control
Ultrasound through the front abdominal wall of the mother penetrate the vein of umbilical cord and
overflow 20-50 ml of erythrocyte mass). This operation improves
Fetal condition and allows prolong pregnancy.
Regular
Observation of pregnant women with rhesus sensitization in specialized
Centers allows you to choose the best time and method of the delivery.
Prevention of elevated body sensitivity - sensitization
Important
The role in the prevention of rees-sensitization is given to family planning.
Guarantee of the birth of a healthy child in a rhesus-negative woman (when
Absence of preceding sensitization during blood transfusions)
is the preservation of first pregnancy.
WITH
The purpose of the prevention of cut-sensitization is used by the drug
Domestic Production - Antiresus-Gamma Globulin. This drug
destroys the remaining after childbirth in the bloodstream
erythrocytes of the fetus, thereby navigating themselves actually
maternal immune response (maternal anti-stercered production
antibodies). Enter this drug is necessary after childbirth, if born
Resh-positive child; after artificial or spontaneous
abortion; After the operation produced in connection with
Emascinal pregnancy. It should be remembered that the effectiveness of this
The drug is largely due to the deadlines of the introduction: when allowed
time to 72 hours is considered not more than 2 hours after
labor or listed above operational interventions.