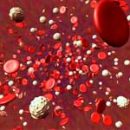
Thrombocytopenia - (from platelets and Greek. Penia - disadvantage) - reducing the number of blood plates in a unit of blood volume. How is the treatment of this disease? The answer to this question you will receive in the article.
Content
What thrombocytopenia is
Thrombocytopenia can be an independent disease or a symptom of a number of pathological conditions (both acquired and hereditary): it may be due to increased destruction of platelets, increased consumption of them or inadequate education.
In most cases, thrombocytopenia is acquired. They are distinguished depending on the pathogenesis and the reasons for damage to platelets or megacariocytes.
 Acquired thrombocytopenia include: immune thrombocytopenia, in which antibodies are formed during hemotransphuses or fall into the body of the fetus from the mother; thrombocytopenia due to the oppression of proliferation of bone marrow cells; thrombocytopenia associated with the somatic mutation of myelopoese predecessors; thrombocytopenia of consumption observed during thrombosis, extensive hemorrhages, expressed splenomegaly; thrombocytopenia, developing due to the replacement of bone marrow tumor, for example, during cancer metastasis in the bone marrow, during hemoblastosis; Thrombocytopenia, due to mechanical damage to platelets in hemangiomas, expressed splenomegaly, in the presence of artificial heart valves, thrombocytopenia with vitamin B12 deficiency or folic acid. In clinical practice, immune thrombocytopenia are most common, associated with the impact on antibody platelets.
Acquired thrombocytopenia include: immune thrombocytopenia, in which antibodies are formed during hemotransphuses or fall into the body of the fetus from the mother; thrombocytopenia due to the oppression of proliferation of bone marrow cells; thrombocytopenia associated with the somatic mutation of myelopoese predecessors; thrombocytopenia of consumption observed during thrombosis, extensive hemorrhages, expressed splenomegaly; thrombocytopenia, developing due to the replacement of bone marrow tumor, for example, during cancer metastasis in the bone marrow, during hemoblastosis; Thrombocytopenia, due to mechanical damage to platelets in hemangiomas, expressed splenomegaly, in the presence of artificial heart valves, thrombocytopenia with vitamin B12 deficiency or folic acid. In clinical practice, immune thrombocytopenia are most common, associated with the impact on antibody platelets.
Select a group of hereditary thrombocytopenia due to the inferiority of platelets, which leads to shortening the duration of their life. In hereditary thrombocytopenia, there is often a change in the various functional properties of platelets, which gives the basis to attribute them to the thrombocytopathy group. Inheritance include thrombocytopenia, due to a platelet membrane defect, combined with a violation of their functional state.
All forms of thrombocytopenia are characterized, as a rule, painless spotted hemorrhages. With most thrombocytopenia, hemorrhages in the skin or various types of bleeding of mucous membranes are noted (gums, nasal, gastrointestinal and others.).
In patients with thrombocytopenia, during blood test, there is a decrease in the number of platelets up to a complete disappearance, a normal or elevated content of plasma blood coagulation factors, a decrease in the consumption of prothrombin, a breakdown of the bloodstream retraction (sometimes there is no retraction). With severe thrombocytopenia in most patients, bleeding time increased. Due to the increased incidence of capillaries associated with the violation of the angiotrophic function of platelets, the samples for the resistance of capillaries, such as the jammed sample, are sharply positive. In the diagnosis of hereditary thrombocytopenia, a morphological analysis of platelets (their value, structure), determination of their functional properties play a significant role.
How the thrombocytopenia is treated
All patients with any manifestations of hemorrhagic syndrome should be hospitalized.
When increasing the number of subcutaneous hemorrhages in the process of observing the patient and / or connection of bleeding, therapy is shown by hormones. Premisone as initial therapy is prescribed in an average daily dose of 60 mg / m2 (which corresponds to 2 mg / kg per day) 3 weeks 3 times a day (600, 1000, 1400), taking into account the daily biorhythm - 2/3 of the daily dose of prednisolone are given In the morning hours.
Upon reaching a complete remission, the prednisiolone dose decreases at 5-10 mg at 3 days until complete cancellation.
If there is a patient serious bleeding, the initial dose of hormones can be 3-5 mg / kg per day for 3-5 days before the gap of hemorrhagic syndrome with the transition is then at a dose of 2 mg / kg per day. Alternatively can be pulse therapy: methylprednisolone 30mg / kg per day for three days (time of infusion - at least 20 minutes) before the gap of hemorrhagic syndrome and increase platelets to a safe level (more than 20,000).
Initial or alternative therapy may be the introduction of intravenous immunoglobulin (IGG in / c). Preparations used: octagam, pentaglobin.
Also during the thrombocytopenia, the motor regime is dramatically limited.
Symptomatic therapy is carried out:
- Angioprotectors - Ditinon;
- fibrinolysis inhibitors - aminocaproic acid 0.2-0.5 g / kg per day;
- Local ways to stop bleeding.
The duration of the disease for more than 6 months indicates a chronic form of the disease, although the likelihood of spontaneous recovery is not excluded, even in a few years, the possibility of a new deterioration (crisis) or continuously recurrent flow.
All patients should be excluded aspirin and other antiagregants and / or anticoagulants. Do not do intramuscular injections. Vaccinations and allergens are excluded (including food), as they can increase the degree of thrombocytopenia. Sport classes must be stopped to prevent the possibility of injury. Swimming in this sense is safer. If the patient leads a fairly active lifestyle, symptomatic therapy is necessary: alternation of cookies of phytotherapy (nettle, yarrow, rosehip, shepherd bag, arnica, etc.) with angioprotectors (ditinon - 1. X 3 R., Magnum from 0.25-0.5 x 1p., Traumel 1T. X 3 R.).
It is necessary to emphasize - treatment should be carried out individually.