What diseases causes staphylococcus? How they manifest? What to treat them? Answers to these questions you will find in the article.
Content
Staphylococci - Extremely common representatives of skin microflora and mucous membranes. As causative agents of infections they were discovered among the first. Staphylococci cause many
infections, including superficial and deep purulent infections, intoxication, urinary tract infection. In the US, they are the leading cause of sepsis, postoperative wound infection and infections
Endoprosthenes. Among the pathogens of hospital infections, they rank second in frequency. except
Togo staphylococci is one of the leading causes of microbial food poisoning.
The most important for humans staphylococcal, causing various diseases, is golden
Staphylococcus - Staphylococcus aureus - persistent, easily acquiring antimicrobial resistance
drugs causative agent infection. Other staphylococci, in particular - epidermal staphylococcus -
Staphylococcus Epidermidis, show a tendency to foreign materials (endoprosthesies) and increasingly
become causative agents of hospital infections, especially in patients with weakened immunity. Other Staphylococcus, Staphylococcus SAPROPHYTICUS, - common pathogen of urinary tract infections.
Staphylococcal toxic shock
Toxic shock - acute, threatening life intoxication, which manifests itself
fever, arterial hypotension, rash, polyorgan deficiency and, at the beginning of the period
recovery, peeling skin. Toxic shock was first described in 1978., but attracted to themselves
Universal attention only after 2 years - due to a large outbreak among women who used
Tampons during menstruation. This disease is a bit common (1 case per 100,000 women
Children age per year). It is possible however, that it occurs more often than diagnosed. Approximately half of cases are not related to the use of tampons and is distributed between men and women of all ages. The clinical picture of toxic shock is always the same, regardless of its reason.
Toxic shock causes produced toxins produced by gold staphylococci. He
More often occurs in young people, as more than 90% of adults have antibodies to causing it
Toxins.
Most often, toxic shock occurs during menstruation, but may develop as a complication of barrier contraception, postpartum period, infected abortion, gynecological operations, skin injuries (including chemical and thermal burns, insect bites, wind oil and operating wounds). After surgical interventions, toxic shock is developing in time from several hours to several weeks. For its occurrence, a clinically pronounced staphylococcal infection is not required, sufficient carriage of staphylococcus producing toxins. Therefore, signs of inflammation at the place of the formation of toxin are not always. On the other hand, toxic shock can develop against the background of staphylococcal muscle infection, bones, joints, respiratory tract.
Toxic shock begins acutely, with high fever, nausea, vomiting, diarrhea, abdominal pain, muscles, throat, headaches. Dizziness alone or when rolling - a sign of reduced blood pressure. In the first 2 days of the disease, a characteristic spotted rash appears, usually generalized. Rash can pass quickly or preserve for a long time. Often there are violations of consciousness. In many cases, redness of the eyes and mucous membranes are noted and swelling, half of the patients - a red strawberry language.
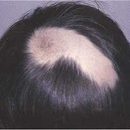
The early symptoms of toxic shock are held within a few days, after which the consequences of arterial hypotension (reduced blood pressure) are the leading manifestations - disorders of the kidney and heart function, massive swelling and T.D. Approximately a week begins peeling of the skin of the body, face, limbs. In the footsteps, palms and fingers, the skin is listed. Frequent complications are often complications - gangrene limbs, muscular weakness, reversible loss of nails and hair, neurological and mental disorders.
Treatment of toxic shock consists in eliminating the focus of infection, infusion therapy and the appointment of antibiotics active in relation to golden staphylococcus. Required audit and washing of fresh operating wounds, even in the absence of signs of inflammation.
More than half of the patients undergoing toxic shock, antitoxic immunity is not produced. Golden staphylococcal carriage in the vagina can carry a permanent or recurrent character, so it is not uncommon and repeated cases of toxic shock.
Ritter disease (Skin Syndrome)
Skin Syndrome (Ritter Disease) Causes Golden Taphilococcus,
producing certain types of toxins. They sick them mostly newborn and children of the younger
Age. After 5 years, scalding skin syndrome is rare, only against the background of severe diseases (for example, renal failure) or immunodeficiency. This is due to the development of antitoxic immunity and, possibly, a decrease in sensitivity to these toxins. Most adults have antibodies to staphylococcal toxins. The development of scaffolding syndrome is preceded by staphylococcal infection, most often - purulent rhinitis.
Syndrome of scratching skin often begins with head pains, cognition, lobs in muscles, possible - vomiting, diarrhea. After that, a red fine-point rash appears - first around the eyes and mouth, then spreads on the body and the limb. Rash is especially expressed in large skin folds. Skin to the touch resembles sandpaper, when touched pain. Frequent edema around the eyes, children - irritability or drowsiness, subfebrile temperature. After a few hours or a day, the detachment of the upper layers of the skin begins. The skin becomes similar to cigarette paper; the slightest pressure (even on externally healthy sites) causes a detachment. After about 48 hours, the deprived surface layer of the skin dried, and peeling begins. The disease lasts about 10 days.
The disease can cause dehydration and sepsis, which is caused by the cause of death.
Treatment includes antibiotics active in relation to staphylococci, infusion
Therapy and thorough care for affected skin.
Food toxicoinfection caused by staphylococcus
The disease begins 2-6 hours after the use of infected food from a sudden appearance of nausea, vomiting, grasp abdominal pain, diarrhea. Food toxicoinfection causes toxins of golden staphylococcus, formed in the disgraced food and having fallen into the gastrointestinal tract. Since the body receives ready toxin, the disease develops quickly. Staphylococcal toxins withstand heating to such temperatures under which staphylococci themselves die. The incidence is quite high; in the summer it is somewhat higher than the rest of the year. The reason most often serves meat dishes and cakes with custard - perhaps because staphylococci, being resistant to high concentrations of protein, salt and sugars, multiply in these products, without experiencing competition. Flashing diseases are usually associated with eating, long stored at room temperature. Food is often seaming due to inventory pollution and non-compliance with personal hygiene by persons preizing it.
Skin and soft tissue infections
Golden Staphylococcus - the most frequent pathogen of skin infections and soft tissues. These infections can be primary or secondary, that is, developing against the background of another disease. Causes them, as a rule, the sick microflora.

A number of infections - from the lungs to severe, threatening life - begins with hair follicles.
Folliculitis - Inflammation of the top sections of the hair follicle - manifests itself with yellowish pustula,
surrounded by a narrow red wedge. To speed up recovery, antiseptics are used; in
Heavy cases may require antibiotics (locally or inside). Furuncul - acute purulent
Inflammation of the hair follicle and the surrounding fabrics. In the center of the furuncule is formed
necrotic rod. Favorite Localization - Buttocks, Face, Neck. When palpation, the furuncle tight and painful. Frequent fever and generality violation. To speed up recovery and avoid the formation of a scar, often requires autopsy and drainage, as well as antibiotics. If the Golden Staphylococcuit is not eliminated, the furunculosis can be repeated. Carbuncoon is formed when merging several boils with the formation of a zone of spilled inflammation of soft tissues. Favorite depth - rear surface of the neck, shoulders, buttocks, hips. The disease occurs with a high fever and a violation of the general condition. It is more common in men - middle-aged or elderly. Opening, drainage and appointment of antibiotics are required. Golden Staphylococcus - the most frequent pathogen of paronymich (inflammation of near-gas tissues).
Golden Staphylococcus causes a bullous impetigo - surface skin infection,
meeting predominantly in children. Under the action of exfoliatins, a detachment takes place
Surface layer of skin and bubbles formation with a diameter of 1-2 cm. The causative agent of the usual (neboral) impetigo, as a rule, serves Streptococcus pyogenes, but in this case staphylococci can cause superinfection. With limited defeat, the local use of antibiotics is sufficient; With a common or leaky with an increase in lymph nodes - antibiotics are prescribed inside.
Felmons - Spilled Inflammation of Subcutaneous Fiber - Staphylococcus Aureus is less common than Streptococcus Pyogenes. Staphylococcal phlegmon usually develops as a wound infection - after injuries and operations, and not with small and inconspicable skin damage. In the treatment of phlegmon, it is advisable to use antibiotics, active both in terms of Streptococcus Pyogenes, and with respect to Staphylococcus aureus. Unlike Streptococcus Pyogenes, Staphylococcus aureus is not a causative agent of face - surface infection of the skin and subcutaneous fiber, the distinctive feature of which serves clear boundaries and raised edges of the affected area.
Respiratory infections
Golden Staphylococcus falls in her legs through blood or in the lungs
Microflora upper respiratory tract. Staphylococcal pneumonia is relatively rare, but heavy
Infection for which breast pain, shortness of breath, intoxication. It almost always occurs in the presence of risk factors (unfavorable epidemiological situation, the carriage of golden staphylococcus in the upper respiratory tract, imminent immunity). Hospitalization, antibiotic therapy, stay in nursing homes and disabled people predispose to the carrier of golden staphylococcus. Most often, staphylococcal pneumonia develops after intubating trachea or viral respiratory infection. Influenza virus contributes to the population of the upper respiratory tract with golden staphylococcus.
Staphylococcal pneumonia can develop with infectious endocarbage of the right heads of the heart
(especially common among injection drug addicts) and purulent thrombophlebitis, often
complicating vehicle catheterization. Pneumonia begins acute - chest pain and shortness of breath. Wets may not be; But on the radiograph of the chest, as a rule, multiple focal shadows are visible - a characteristic sign of such pneumonia. Empiama - a common consequence of staphylococcal pneumonia, and without that giving a lot of complications.
Golden Staphylococcus sometimes the main microorganism detected in the strokes from the mouth
Patients of angina, especially children. Staphylococcal angina may be accompanied by Scarlantine-like
rash and severe intoxication (as with toxic shock). Intoxication is typical for
Staphylococcal tracheitis. Golden Staphylococcus - a frequent pathogen of chronic sinusitis, which, as a rule, arise as a result of illiterate antimicrobial therapy, leading to the formation of antibiotic antibiotic.
Staphylococcal infections of the central nervous system
Golden Staphylococcus falls into the central nervous system through blood or from nearby fabrics. It is one of the main causative agents of brain abscesses, especially those that are formed as a result of septic embolism. This usually happens with infectious endocardius of a mitral and aortic valve. Similar abscesses - often small, numerous, scattered throughout the brain. The brain abscess can develop as a result of the spread of infection with the appropriate sinuses of the nose (frontal, wedge-shaped, lattice maze) or soft tissues (after penetrating injuries and surgical interventions). Purulent meningitis can develop on the background of staphylococcal abscesses of the brain or be the result of the phantom of staphylococcus in blood. In the latter case, abscesses do not find abscesses.
Golden Staphylococcus more often than other microorganisms causes other intracranial bulk
infectious processes. Subdural empieme - as a rule, the result of the distribution of staphylococci from the focus of osteomyelitis bones of the skull, sinusitis, wound infection (during operations and injuries). Subdural empieme is often accompanied by meningitis, epidural abscess, thrombophlebitis of the superficial veins of the brain and thrombosis of solid cerebral sinuses. Basic signs: fever, headache, vomiting, symptoms of brain shell irritation. As the infection progresses, the edema develops, and often the heart of the brain, there are disorders of consciousness, epileptic seizures, focal neurological symptoms. The patient's condition can deteriorate very quickly. Urgent surgical intervention, drainage and antibiotics are needed.
Golden Staphylococcus - the most common pathogen of spinal epidural abscess,
which usually develops as a complication of osteomyelitis of the spine. Characteristic fever, pain in
back, root pain, weakness in the legs, disorders of defecation and urination. Sometimes sick
complains of weakness or difficulties in walking, and there are no objective signs of lesion yet. The main danger represents the destruction of the brain tissue due to the thrombosis of the veins or the compression of the spinal cord. If you do not recognize the spinal epidural abscess on time, irreversible consequences are possible, for example, paralysis. In the absence of focal neurological symptoms, an attempt to conservative treatment with antibiotics is admissible, but more often the urgent decompression of the spinal cord is required by laminectomy and drainage of the infection. Intracranial epidural abscess develops as a complication of sinusitis, injuries, tight trees. The clinical picture consists of symptoms of osteomyelitis of adjacent bones, intracranial volumetric process, brain edema and often - secondary infection of subdural space. For rescue of life, an emergency surgical intervention is necessary.
Finally, golden staphylococcus serves as the most common cause of thrombophlebitis of surface veins
brain and thrombosis of solid cerebral sinuses - typical complication of sinusitis,
Mastoiditis, infections of soft fabrics. The clinical picture depends on the underlying disease and those anatomical structures that are in contact with the affected vein or sine. Possible disorders of consciousness, paralysis, parish.
Urinary tract infections caused by staphylococcus
Golden Staphylococcus - an infrequent cause of urinary tract infections. Primary
Staphylococcal infections almost always occur after cystoscopy, installation of constant urinary
catheter and other interventions. In other cases, the presence of golden staphylococcus in the urine, even in small quantities, gives reason to suspect the population of staphylococcus in the blood and in the kidneys (with the formation of an abscess or without it). The reason is often served staphylococcal endocarditis.
Endovascular infections caused by staphylococcus

Golden Staphylococcus - the most common pathogen of acute infectious endocarditis, including endocarditis of prosthetized valves. Staphylococcal endocarditis is a sharp feverish disease with a duration of no more than a few weeks. By the time of appeal for medical help, severe complications often manage to develop - meningitis, brain abscesses and abdominal cavities, septic peripheral arterial embolism, heart failure due to valve deficiency, myocardial abscess, purulent pericarditis. Mitra or aortic valve (either both) is affected by most. The exception is the staphylococcal endocarditis in injecting drug addicts, which most often suffers from a three-rolled valve. Characteristic features of the disease: noise in the heart, eyemination in the eyes, subnogric hemorrhages and hemorrhagic rash on palms and soles.
Staphylococcal endocarditis is accompanied by high mortality (40–60%), so antimicrobial
therapy should be started immediately.
Complications requiring valve prosthetics develop approximately half of the patients, so the cardiac surgeon consultation should be held as soon as possible. Sendance with the operation worsens the forecast. Endocarditis of the right heart departments is found mainly in injection drug addicts and in patients who were conducted by vehicle catheterization. It is often complicated by the septic embolism of the branches of the pulmonary artery, but the rest gives less complications than the endocarditis of the left departments. Forecast with endocarditis of the right hearts of the heart is better, and the testimony for valve prosthetics occurs less frequently than with the endockarization of the left departments. For cure, there is enough two-week antimicrobial therapy courage. On the contrary, with staphylococcal endocarbage of prosthetized valves (as early, so and later), the testimony for their replacement occurs almost always.
The tendency of golden staphylococcus attached to damaged tissues makes it the main
causative agent and other endovascular infections. They arise when driving Golden Staphylococcus
blood in damaged vessels. In particular, an examination of atherosclerotic plaques in large
Arteries lead to the development of septic aneurysm. Immediate distribution
Infections from adjacent focus. In this way, an infected false aneurysm occurs after vessels and purulent thrombophlebitis during veins catheterization. Staphylococcus infection affected
Atherosclerosis of the artery (most often it is an abdominal aorta or iliac artery) with development
Aneurysms - the hardest complication. It is accompanied by a large amount of staphylococcus
blood and ends with a gap aneurysm with profuse bleeding. Without excision amazed
Section of artery and shunting The cure is almost impossible.
Purulent thrombophlebitis is also accompanied by the emission of a large number of staphylococcus in the blood and
intoxication, but versions of veins are observed significantly less. At the same time you need to remove infected
Trombo or excised Vienna. If it is technically difficult, an attempt is justified by conservative treatment
Antibiotics and anticoagulants.The complications of staphylococcus falling into the blood include abscesses
Abdominal cavity and brain, meningitis, purulent arthritis, osteomyelitis, infectious endocarditis, septic aneurysm.
Staphilocontal infections of muscles, bones and joints
Golden Staphylococcus - the main causative agent of acute osteomyelitis in adults and one of the most frequent in children. Acute osteomyelitis develops as a result of the bore in the blood of staphylococci (especially in damaged bone) or their distribution from the adjacent focus of infection. In adults, hematogenous osteomyelitis is most often striking the body of the vertebrae, in children - long tubular bones. In acute osteomyelitis, adults in the clinical picture are a violation of a general condition and pain in the field of lesion, which appears not immediately. Acute osteomyelitis usually requires antimicrobial therapy for 4-6 weeks.
Chronic osteomyelitis is also often caused by golden staphylococcus. It develops at the place of operating wounds, injuries, in violation of blood supply to the bone. Chronic osteomyelitis is straightely different from most other staphylococcal infections, which are characterized by a rapid flow. He can remain asymptomatic years and even decades, and then give a spontaneous recurrence with pain, the formation of fistulas and the allocation of pus. In chronic osteomyelitis, surgery is needed with subsequent long-term antimicrobial therapy.
Its features has osteomyelitis after prosthetic joints, immersion and outdoor
Osteosynthesis. The prosthetized joint infection is manifested by pain, fever, swelling and
restricting its mobility. Alone antibiotics for cure, as a rule, is not enough. When sepsis, stubborn bacteremia, clinical or radiological signs of the prosthesis instability shown its removal. If the removal of the prosthesis is extremely undesirable, carry out a course in / in antimicrobial therapy followed by the transition to long-term reception of drugs inside. Metal structures infected with staphilococci, fixing bone fragments, should also be deleted, but this procedure is often postponed on as long as possible time to give time to the fracture.
Golden Staphylococcus - the main causative agent of purulent arthritis in adults. To the disease
Injecting drug addiction, rheumatoid arthritis, treatment with glucocorticoids (systemic or intra-articular administration), penetrating the injury, osteoarthritisosis. Most often, the knee, hip and sacriven-iliac joints suffer. In addition to / in antimicrobial therapy, drainage is needed - by multiple punctures, arthroscopic or open surgical intervention. Insufficient drainage leads to a violation of the mobility of the joint. Golden Staphylococcus is also the main causative agent of purulent bursitis.
Caused by golden staphylococcus, purulent myozit in moderate climate is rare. One of
Species - PSOs-abscess. Its reason is the drift by blood infection or its immediate
Spreading on the ileum-lumbar muscle at osteomyelitis of the spine. He manifests itself
pain in extension of legs in hip joint and fever. Pso-abscess often gives in
percutaneous drainage, in other cases resort to surgery. Rest
Forms of staphylococcal purulent mositis are found almost exclusively in the tropics (the so-called tropical piomyosis). Almost all cases develop on the background of diabetes mellitus, alcoholism, hemoblastosis or immunosuppressive therapy.