To date, the brain injury (CMT) is one of the most common types of neurological pathology and is a significant medical and socio-economic problem for all segments of the population.
Content
In developed countries, there is a steady growth of neurotraumamism. So in the countries of Europe, 150 is registered annually–300 cases of CHMT per 100 thousand. Population. In the US, only 2003. Noted more than 1.5 million CMT. In Russia, this figure reaches 4 cases per 1 thousand. Human. The most important problem in the medical terms is that a significant number of victims are subsequently developing the so-called consequences of the postponed CMT, often interpreted within post-traumatic encephalopathy. Among the most common syndromes that determine the level of socio-household adaptation and the quality of life of patients are intellectual-unique violations. Post-traumatic cognitive disorders are isolated in 29.4% of all patients with the consequences of CHMT, and in combination with other syndromes — y 35.7%. In general, among the consequences of the postponed CMT cognitive disorders as syndrome are found in 65.1% of cases.
The pathogenesis of the development of post-traumatic cognitive disorders is very complex and multifaceted. As the main factors that can lead to the formation of a cognitive deficit in the acute period, we consider both direct mechanical damage to the brain tissues and the mediated effect of certain pathophysiological processes arising from the CHT, such as the swelling of brain swelling, disruption of liquor, hemodynamics and Dr. At the same time, it is known that in terms of cases of disorder of intellectual-meal functions, a long time is preserved or is a persistent character. In other patients, they appear in the distant period of injury and have a distinct trend towards progression. The mechanism of occurrence of such violations remains not studied in the remedy. The data obtained suggests that pathological factors affect the nervous cell in the acute period, contribute to the emergence of a cascade of biochemical shifts in neurons, leading to the development of dystrophic processes and reduce the effectiveness of synaptic transmission.
Ultimately, there is a violation of information dissemination processes in neuronal networks, which is considered as one of the main aspects of the formation of cognitive violations. A number of researchers note a certain similarity of the pathogenetic mechanisms for the development of cognitive disorders at CMT and vascular brain lesions. In addition, a possible role of brain injury is shown as a launcher of neurodegenerative diseases, in particular Alzheimer's disease. Currently, several pathophysiological processes playing a significant role in the formation of post-traumatic cognitive disorders.
One of these processes is the development «Glutamate exaitotoxicity». In physiological conditions, glutamate acts as one of the most important exciting mediators of the central nervous system, participating in the implementation of the processes of neuronal plasticity and the integrative functions of the brain. A significant amount of glutamanthergic receptors is observed in the cerebral cortex and hippocamp. At the same time, with pathology, excess glutamate emissions are observed, which in these conditions has a toxic effect on neuronal structures, which contributes to the activation of the glutamate-calcium cascade reactions, leading to an uncontrolled increase in the concentration of intracellular calcium, which has a negative effect on cell energy supply. It is shown that under the conditions of ischemia in tissues there is a significant increase in the level of formation of free radicals, which also contributes to excess intracellular accumulation of calcium.
The brain is very sensitive to the action of free radicals. In the conditions of the predominance of oxidant systems over antioxidant, the formation of the so-called oxidant stress. In this case, the hydrolysis of phospholipase is activated and the cell membranes are degradation, including mitochondrial. The elimination of emerging disorders is a prerequisite for successful patient management with post-traumatic cognitive impairment. With these positions, it is appropriate to the appointment of such a drug as a noopept with such properties. Noopept — N-phenyl-acetyl-L-prolyglycine ethyl ester — New domestic original dipeptide created in pharmacology. IN.IN.Zasakova Ramne. According to the data obtained in the course of experimental studies, NOPEPT has nootropic and neuroprotective properties. The drug in its structural conformational characteristics is similar to piracetam and vasopressin. The development of this drug was carried out as part of the existing idea that some regulatory peptides have a significant impact on the mechanisms of memory and training.
The basis of the explanation of the action of Noopept is a hypothesis that the base drug of this group of piracetam is an analogue of a peptide ligand to specific nootropic receptors, similar to its characteristics with vasopressin metabolites. Noopept is beneficial from vasopressin because it is capable of showing activity with systemic, including oral administration. During the studies, the high bioavailability of the drug for brain tissues was shown, as well as its low toxicity. Study in the experiment on laboratory animals made it possible to establish that the use of drug dosages, from 2 to 20 times higher than nootropic, does not cause damage to the internal organs, does not have significant violations of hematological and biochemical indicators. When conducting a number of clinical studies, high safety of the drug and its good tolerability is also shown. In the course of the research, it was found that noopept has a comprehensive mechanism of action.
First, it has a nootropic effect associated with the fact that one of the active metabolites of Noopept is cycloprolglycine, which, in its structure, is similar to an endogenous cyclic dippotide, which has anti-informic activity.
Secondly, Noopept is able to increase the stability of the cerebral tissue to damaging impacts, such as injury, hypoxic, electrosuscular and toxic lesion, which characterizes the neuroprotective effect of this drug. Thirdly, it is shown the possibility of a noopept to prevent in the conditions of the actions of the toxic concentrations of glutamate and the active forms of oxygen death of neurons in the body of the cortex of the cerebral cortex and cerebellum. In addition, the experiment revealed the ability to reduce the toxic effect of B-amyloid, enhance the production of anti-mylide antibodies, modulate the operation of cholinergic receptors, as well as stimulate the expression of neurotrophic factors (BDNF and NGF) in the cerebral cortex and hippocamp.
The relevance of the problem of post-traumatic cognitive violations, the validity of the use of noopept, taking into account the presence of an application points at the neurochemical level under the consequences of the CHT, as well as the preliminary, including the experimental and clinical efficacy of the drug was the reason for this study.
The purpose of the study was to evaluate the effectiveness, as well as the safety of the use of the drug Noopept in patients with light post-traumatic cognitive disorders. The study was conducted on a specially developed protocol and complied with all the requirements of appropriate clinical practice (GCP) adopted in the Russian Federation. The study included patients that meet the criteria for inclusion, after the mandatory signing of informed consent.
30 patients aged 19 participated in the study–66 years old (average age 33±10.3 years), who suffered a CHHT (concussion or injury brain of a light degree) at least 6 months ago and having a disruption of intellectual-meal functions associated with this state corresponding to the criteria for moderate cognitive disorders syndrome. All patients corresponded to the criteria for the syndrome of moderate cognitive violations, and their cognitive disorders were originally evaluated in 25 or more points on the MINI-MENTAL STATE Examination scale (MMSE).
Exceptions criteria from research were: the presence of concomitant heavy or unstable somatic diseases that threaten the life of the patient, the presence of clinically significant other (except for the syndrome of moderate cognitive violations with the consequences of the CHF) neurological or mental disorders, the presence of a coarse motor or sensory defect or other disorders that made it difficult It would be carrying out a neuropsychological study or other studies provided for by the Protocol, a history of stroke or discirculatory encephalopathy stage III, simultaneous conducting therapy with other vasoactive, metabolic or psychotropic drugs with proven cognitive-stimulating effect, intolerance to the drug under study, pregnancy and lactation period.
When performing work to objectivate the data obtained were applied
The following methods:
1) assessment of neurological status;
2) A brief scale of mental status — MMSE;
3) Hamilton scales to assess depression;
4) Test battery for frontal dysfunction — FRONTAL ASSESSMENT BATTERY (FAB);
5) watch drawing test;
6) Test 10 words;
7) Trial Schulte;
8) rating scale of a general clinical impression of change — Clinician’S Interview Based Impression of Change Plus (CIBIC PLUS);
9) Neuroviasualization methods: Computer or magnetic resonance tomography.
Assessment on a scale of a general clinical experience provided for an assessment of the patient's condition to therapy and evaluation of the severity of changes in the background of treatment. The attending physician before the start of therapy made an assessment of the patient's condition on the basis of an analysis of disorders on a 7-point scale, estimating the clinical picture of the disease, monitoring the patient, the state of the mental sphere of the patient, the behavior, the state of socio-domestic functions.
At the beginning of the study, a screening visit was carried out, on which the patient's compliance was determined by the inclusion criteria. Then, in the case of patient conformity, the protocol was signing informed consent. This visit also evaluated the results of electrocardiograms, laboratory and neurovalization methods of research. After that, neurological status was estimated, basic neuropsychological testing was carried out in order to determine the initial level of the state of cognitive functions.
Starting with the next day of the screening visit, patients received a noopept for 10 mg 2 times a day for 60 days. In the future, the evaluation of the effectiveness of therapy was carried out on the 30th and 60th days of treatment. The plan of the events is presented in the table.
In our study, the average period after the suffered injury was 7±3.8 years. All 30 patients who have entered the study, originally had light violations on the scale of the general clinical impression of the change (Cibic Plus). During a screening visit, all examined patients presented complaints about reducing memory, concentration of attention, reducing the effectiveness of performing daily activities, general weakness, increased fatigue. In addition, some of the patients presented other complaints: on headache (43.3%), difficulties with planning various activities (40%), sleep disorder (26.7%), mood instability (23.3%). During the neurological examination of gross violations was not detected. In 53.3% of patients, there was scattered symptoms in the form of isolated microsimptoms, 13.3% — Light coordinator violations. At the same number of observed bilateral pathological plastic reflexes (Rossolimo, Vartenberg). All patients had signs of asthenic syndrome. 53.3% have observed signs of vegetative-vascular instability.
The study of cognitive functions of patients conducted in the dynamics showed that, by the results of the MMSE scale, reliable differences with the initial level were shown 30 days after the start of treatment. In particular, before the admission of the drug, the average score was 26.5±0.94; 1 month from the beginning of therapy — 27.6±0.99 points (p<0.01). At the same time, 60 days from the beginning of therapy, the average score on this scale was 27.7±1.09, which characterized the absence of further reliable improvement (P>0.05) and only a tendency to reduce cognitive disorders was displayed. The dynamics of neuropsychological indicators on the MMSE scale is presented in rice. one.
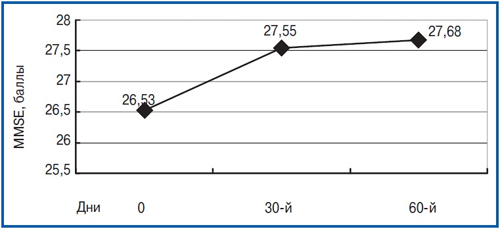
Picture 1
Interesting was the fact that in the structure of the MMSE scale, the most significant improvement in the indicators was obtained by Subshkale «Attention», characterizing to a certain extent the state of neurodynamic processes suffering from TBMC (P<0.01), as well as on Subshkale «memory» (R<0.05). On the battery scale of tests to evaluate the frontal dysfunction of FAB reliable differences over the observation period in the dynamics was not available (on the initial visit — 15.9±0.78 points, 60 days later — 16.8±0.87, p = 0.27). The test of the drawing test of the clock with a 10-point estimate on the source visit is usually estimated at 9–10 points and against the background of the treatment of significant changes did not undergo. Of course, the data obtained on the basis of the evaluation of the sample results of the Schulte, which was performed on all 3 visits. Comprehensive estimated sample using 5 consecutively presented patients tables most fully allows you to characterize such neurodynamic changes as a deterioration in the concentration of attention, increased depletion of mental processes and instability attention. These changes to a certain extent were characterized by most patients on screening visits. The average test time for each of the five presentations in the first visit was 45.5±6.24 S. After 2 months after the start of therapy, the time decreased to 40.2±5.20 s, which characterized a significant improvement in the concentration of attention (p<0.05). The dynamics of the sample time of the Schulte is presented in rice. 2.
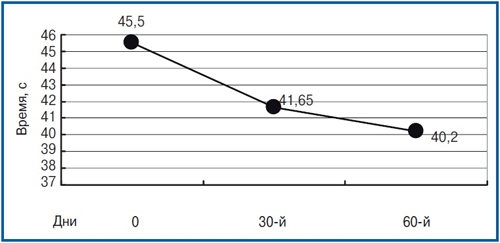
Figure 2
As can be seen from the graph in rice. 2, the most significant reduction in the time spent on the execution of samples was shown by patients 30 days after the start of therapy. Recognizing positive dynamics also persisted over the 2nd month of the drug and was characterized by an even more pronounced decrease in the test time with a less significant stabilization of improvement than on the MMSE scale.
Assessment on a scale of a general clinical experience provided for an assessment of the patient's condition to therapy and evaluation of the severity of changes in the background of treatment. The attending physician before the start of therapy made an assessment of the patient's condition on the basis of an analysis of disorders on a 7-point scale, estimating the clinical picture of the disease, monitoring the patient, the state of the mental sphere of the patient, the behavior, the state of socio-domestic functions.
At the beginning of the study, a screening visit was carried out, on which the patient's compliance was determined by the inclusion criteria. Then, in the case of patient conformity, the protocol was signing informed consent. This visit also evaluated the results of electrocardiograms, laboratory and neurovalization methods of research. After that, neurological status was estimated, basic neuropsychological testing was carried out in order to determine the initial level of the state of cognitive functions.
Starting with the next day of the screening visit, patients received a noopept for 10 mg 2 times a day for 60 days. In the future, the evaluation of the effectiveness of therapy was carried out on the 30th and 60th days of treatment. The plan of the events is presented in the table.
| Research methods | I | II | III |
| Background | 30th day | 60th day | |
| Mental Status Assessment Collection (MMSE) | V | V | V |
| Evaluation of frontal dysfunction (Fab) | V | V | |
| Test drawing hours 10 – Palleal estimate | V | V | |
| Scale of general clinical impression (CGI) | V | V | |
| Test 10 words | V | V | |
| Sample Schulte | V | V | V |
| Hamilton scale | V | ||
| Evaluation of undesirable phenomena and side effects | V | V |
Figure 3
In our study, the average period after the suffered injury was 7±3.8 years. All 30 patients who have entered the study, originally had light violations on the scale of the general clinical impression of the change (Cibic Plus). During a screening visit, all examined patients presented complaints about reducing memory, concentration of attention, reducing the effectiveness of performing daily activities, general weakness, increased fatigue. In addition, some of the patients presented other complaints: on headache (43.3%), difficulties with planning various activities (40%), sleep disorder (26.7%), mood instability (23.3%). During the neurological examination of gross violations was not detected. In 53.3% of patients, there was scattered symptoms in the form of isolated microsimptoms, 13.3% — Light coordinator violations. At the same number of observed bilateral pathological plastic reflexes (Rossolimo, Vartenberg). All patients had signs of asthenic syndrome. 53.3% have observed signs of vegetative-vascular instability.
The study of cognitive functions of patients conducted in the dynamics showed that, by the results of the MMSE scale, reliable differences with the initial level were shown 30 days after the start of treatment. In particular, before the admission of the drug, the average score was 26.5±0.94; 1 month from the beginning of therapy — 27.6±0.99 points (p<0.01). At the same time, 60 days from the beginning of therapy, the average score on this scale was 27.7±1.09, which characterized the absence of further reliable improvement (P>0.05) and only a tendency to reduce cognitive disorders was displayed. The dynamics of neuropsychological indicators on the MMSE scale is presented in rice. one. Interesting was the fact that in the structure of the MMSE scale, the most significant improvement in the indicators was obtained by Subshkale «Attention», characterizing to a certain extent the state of neurodynamic processes suffering from TBMC (P<0.01), as well as on Subshkale «memory» (R<0.05). On the battery scale of tests to evaluate the frontal dysfunction of FAB reliable differences over the observation period in the dynamics was not available (on the initial visit — 15.9±0.78 points, 60 days later — 16.8±0.87, p = 0.27). The test of the drawing test of the clock with a 10-point estimate on the source visit is usually estimated at 9–10 points and against the background of the treatment of significant changes did not undergo.
Of course, the data obtained on the basis of the evaluation of the sample results of the Schulte, which was performed on all 3 visits. Comprehensive estimated sample using 5 consecutively presented patients tables most fully allows you to characterize such neurodynamic changes as a deterioration in the concentration of attention, increased depletion of mental processes and instability attention. These changes to a certain extent were characterized by most patients on screening visits. The average test time for each of the five presentations in the first visit was 45.5±6.24 S. After 2 months after the start of therapy, the time decreased to 40.2±5.20 s, which characterized a significant improvement in the concentration of attention (p<0.05). The dynamics of the sample time of the Schulte is presented in rice. 2. As can be seen from the graph in rice. 2, the most significant reduction in the time spent on the execution of samples was shown by patients 30 days after the start of therapy. Recognizing positive dynamics also persisted over the 2nd month of the drug and was characterized by an even more pronounced decrease in the test time with a less significant stabilization of improvement than on the MMSE scale.