In the treatment of pleurisites, several basic methods allocate. Treatment of the disease begins with the appointment of drugs that have anti-inflammatory effects and influence on the causative agent. For evacuation of exudate, pleural puncture is held.
Content
Pleurrites - inflammation of the sheets of pleura with the formation of fibrin (dry, fibrinic pleurisy) on their surfaces) or a cluster in the pleural region of exudate of various nature (exudative pleurisy).
The main treatment of pleuritic
Treatment of the main disease, the impact on the cause of the disease often leads to the elimination or decrease in the symptoms of pleurite. Distinguish the pleurisites of infectious and noncommunicable etiology.
Infectious pleurisites are caused by bacterial pathogens (pneumococcus, staphylococcus, streptococcus), viruses, rickettsia, mycoplasmas, fungi, simplest (Amebiaz), parasites (echinococcosis), tuberculosis, syphilis, brucellosis, causative agent of abdominal typhoid. The most often infectious pleurisites are observed with pneumonia of various etiology and tuberculosis, but can occur and isolated.
The causes of the pleurisites of non-infectious nature are tumors, diseases of connective tissue, rheumatism, injury and operating interventions, pulmonary artery thrommbolism and light infarction.
If the pleurisy has tuberculosis, then specific anti-tuberculosis therapy is performed; With pneumonia, appropriate antibacterial therapy is carried out; If systemic connecting tissue diseases are diagnosed, immunodepressants (glucocorticoids and cytostatics) are carried out.
If it is not possible to install the etiology of exudative pleurite, it is regarded as an independent disease and prescribe antibacterial therapy, as with acute pneumonia.
Anti-inflammatory therapy pleuritic
Anti-inflammatory tools contribute to the fastest relief of pleuritis, have a painful effect. Non-steroidal anti-inflammatory agents are prescribed (acetylsalicylic acid - 1 g 3-4 times a day, voltar or indomethacin - by 0.025 g 3 times a day and others.).
The desensitizing agents use a 10% calcium solution chloride on 1 tablespoon 3 times a day and other drugs.
With dry pleurisites and severe painful cough prescribed anti-shields (Dionin, codeine of 0.01 g 2-3 times a day and others.).
Evacuation of exudate from pleural cavity
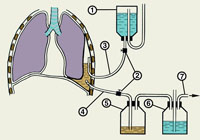 The evacuation of the exudate with the help of pleural puncture has two goals: preventing the development of empya and the elimination of functional disorders associated with the compression of vital organs.
The evacuation of the exudate with the help of pleural puncture has two goals: preventing the development of empya and the elimination of functional disorders associated with the compression of vital organs.
Pleural liquid should be evacuated with large exudates causing shortness of breath, heart offset or if the border of stupidity comes from the front to the second rib. You should delete simultaneously not more than 1.5 l liquid to avoid collapse. In terms of the above indications, pleural punctuation is made even in the early period of exudative pleuritis.
In other cases, pleural puncture with the removal of exudate is better carried out in the stabilization phase or even resorption, since the early evacuation of effusion leads to an increase in negative pressure in the pleural cavity, which contributes to the accumulation of exudate. With an exudative pleurisite of non-specific infectious etiology after removal of the exudate, it is advisable to introduce antibacterial agents to the pleural cavity.
When developing acute empy, the pleura is required to remove the purulent exudate, followed by the introduction of antibiotic pleura in the cavity.
Chronic emmps of pleura are treated operational way.
Correction of violations of metabolic processes
These events are performed with an exudative pleuriste and empy. An intravenous drip infusion of hemodesa, ringer solution, 5% glucose solution is prescribed with a disinfective purpose.
For the correction of protein deficit, a 150 ml of a 10% albumin solution is transfused 1 time in 2-3 days 3-4 times, 200-400 ml of native and freshly frozen plasma 1 time in 2-3 days 2-3 times, intramuscularly 1 ml of retabular 1 is introduced Once every 2 weeks, 2-3 injections.









