Acne (acne) is a disease of the hair follicles and a sebaceous gland, which is found in 80% of adolescents and young people. Among the various clinical varieties of acne, vulgar acne are most often found.
Content
The main factors of the development of acne
- Lipid imbalance.
- In patients with acne marks excess skin formation.
- Participation of microorganisms.
Only 3 groups of microorganisms are the cause of the inflammatory process in the sebaceous glands:
- P.Acne
- Staphylococcus Epidermidis and other kokki
- Lipophilic yeast genus PityRosporum (P.OVALE ET ORBICULARE).
These microorganisms are always present in the comedones (eels). They are
constantly on the surface of the healthy skin of the face and are part
Normal microflora.
In patients acne, a combination of yeast-like (P.ovale) I
Bacterial Flora (P.ACNE). These pathogens lead to blockage
The mouth of the gland.
Hormonal violations
Considering that vulgar acne is usually
appear in the pubertal period when actively start
Functioning sex glands, a significant role in the pathogenesis of acne
Associates sex hormones. Acne arise in women with violation
menstrual cycle with syndrome hyperandrode, with long reception
Androgen or Anabolic Hormones.
A significant role in the pathogenesis of acne plays hereditary
predisposition (genetically deterministic type of secretion of silent
glands and congenital endocrine pathology. Among possible factors
Pathogenesis – Significant reduction in the content of zinc in blood serum
Patients acne and state of immune status.
Manifestations of disease
The most common vulgar or
Youth acne, which are found in 80% of persons aged 15–24 years old.
Character disease the appearance on the face (less often – On the chest I
the appearance on the face (less often – On the chest I
back) comedones, small up to 5 mm in the diameter of pimples bright–red
colors. Rash, allowing, leave pigmentation, less often –
Surface rolls. Salo waste improved, the skin is characteristic
Bold glitter, hair is also fat, perhaps a small breakdown.
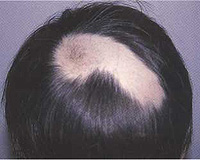
The number of comedones may increase, the mouth of the hair follicles
expand and gap. Comedones arise not only on face, back and
chest, but also in the ear regions, on the scalp.
The inflammatory response around the comedon becomes more pronounced,
Major deep deplete inflammatory nodes are formed. So arise
Inductive acne.
In a few weeks, the nodes are revealed with the formation of the cavity, from
which is distinguished by the drum pus – Phlegmosny acne. After healing
remain deep disfiguring skin scars.
The most common form with pronounced inflammation is
Conglobal acne. They are characterized by the appearance on the back, chest and
The face of large nodes located deep in the skin. Nodes can
Reach 1.5–2 cm in diameter. Such nodes are extremely painful. Merging,
The nodes form conglomerates, abscesses may occur, after opening
which remain long-to-do ulcers, and subsequently – Rough
Scars with jumpers and fistula strokes.
One of the rare variants of inflammatory acne, in which
There is an acute transformation of typical inflammatory acne in extremely
pronounced destructive inflammation, are lightning acne. IN
Mainly suffer from young men. Multiple pains appear
ulcerations with necrosis inflammatory units scattered
Gnoves, located against redness. The process is accompanied
Fever, pain in the joints. Healing occurs with the formation of coarse scars.
Faceproof is quite rarely found – sharp–Inflammatory I
Hard acne. PODERAME FACE MOTHERSHIP TO THE YOUNG
Women who suffered emotional stress or previously received androgens
about endocrine diseases. Dermatosis is characterized by sudden
start and rapid progression. All patients process
Localizes in the central part of the face, in the forehead, temples,
Chin. There is a pronounced swelling of a face with a blue skin tinge, and
in 1–2 days – Painful furuncopod-like nodal rashes,
Reminded konglobal acne, large (more than 5 mm) Gnoves.
Treatment of acne
For the treatment of various forms of acne, a variety of techniques are used, the choice of which depends on a particular patient.
Food factors, various types of food, diet do not matter to develop acne and selection of therapy.
Outdoor therapy does not affect the formation of skin saline. Various
funds, detergents can only temporarily reduce the amount of skin
Sala. However, when using cleansing agents should not be resorted to
exfoliating drugs that can cause skin irritation
Pokrov, trauma.
Comedonal acne
Unreleased comedones – The earliest
Disease manifestation (often in adolescence). Treatment, as
The rule is prophylactic, and includes external means,
Reducing the formation of comedones and the overwhelming development of pathogenic
Flora. Means of choice – Salicylic acid preparations, funds,
containing sulfur, azelain acid, retinol palmitate, tertinoin,
Adapalen, Isotretinoin, benzoyl peroxide.
Teratinoin – high remedy that slows down
Deskvamational process and reduces the formation of microcomedones and
Comedonov. The drug is used in various concentrations and forms:
cream 0.025%, 0.05%, 0.1%; Gel 0.01% and 0.025%. With good
Tritinoin portability is used 1 time per day for affected areas,
Starting with a smaller concentration, followed by the transition to the greater
Cocentration.
Azelainic acid is used in the form of 20% cream 2 times a day on
Problem areas of the skin as a highly efficient means and
Intenuation of tertinin and other drugs. Azelain Acid
Reduces activity oxidative–Recoveful processes I
Number of polyunsaturated fatty acids (for example, arachidon),
destructive effect on P.Acne. Azelainic acid also reduces
Post-inflammatory hyperpigmentation. Antimicrobial I
The anti-heratinizing effect of azelic acid is associated with
Inhibition of protein synthesis.
Both tertinoin and azelainic acid apply within a few months before clinical remission.
Inflammatory forms acne
Light form
When treating a light form of comedenal acne with
An insignificant amount of guns is appropriate to use
Outward alcohol solutions containing salicylic acid, resorcin,
Antibiotics, benzoyl peroxide, ointment with antibiotics. Serious preparations,
salicylic acid, resorcin possess exfoliating and
Antibacterial effect. Means including niacinamide and
A–Hydroxy acids are also quite effective in external therapy.
Gel benzoyl peroxide or solution 1–10% applied 1 time in
Day for 2–3 weeks. The preparation has keratolitical,
deskvamative action, improves tissue oxygenation, leads to
the formation of various forms of active oxygen, destructive effect on
P.acne, suppressing their height. However, benzoyl peroxide does not have a pronounced
anti-inflammatory activity and most rationally use it
3% solution in combination with 3% erythromycin or 7% solution with glycolic
acid.
External antibacterial therapy includes erythromycin,
Tetracyclined, Lincomicin Mazi, Clindamycin. Antibiotics in the form
Outflows are applied 2 times a day. They suppress reproduction P.Acne and others
bacteria.
However, the greatest therapeutic effect is achieved during a combination
benzoyl peroxide and erythromycin ointment that are applied to the skin
covers for a long time before reaching the clinical effect, t.E. before
termination of the appearance of even single papulese and pustular
rash.
Retinoye ointment is also applied for a long time on the plots affected by acne.
It should be remembered: various derivatives of tertinin and retinol can not
use with exfoliating means and with high insolation, in
Combined with UFO–irradiation. With fat seborrhea spend
Preventive therapy, including cryoissage, cleansing and
Exfoliating funds, comedon extraction.
Heavy form
For the treatment of heavy forms of acne with pronounced
Pustilization, destruction of fabrics, heavy cystic and valuable
The process uses a combination of systemic and external therapy.
The exception is isotretinoin, used as monotherapy.
Estrogen, androgens, Spironolactone, Isotretinoin include systemic means.
Women with long-term acne, with ineffectiveness
Antibacterial therapy and outdoor use of tertinine, prescribe
Estrogen and Androgen. At the same time, the defining factors are
Menstrual Cycle Violation, Hisutism, Hypertrichoz, Adrenal
or ovarian hyperandrode. Androgens and estrogens provide
Therapeutic effect with acne by influencing skin saline
and the state of the sebaceous glands.

Diana-35 is prescribed only to women of reproductive age when
The presence of hormonal disorders and ineffectiveness of ordinary therapy.
Spironolactone is used as antandrogen, 100–200 mg per day.
It can have an effect in small doses – 25–50 mg. A drug
affects steroidogenesis in adrenal glands and germ glanes. A course of treatment
spend several months and also apply only in women. Wherein
The amount of skin and pathological elements is sharply reduced.
When pregnancy, spironolactone therapy is contraindicated.
Simultaneously with spirironolakton, it is possible to use other
anticoned tools, as well as oral contraceptives that
prescribe women with ovarian hyperandrogen. Oral
Contraceptives reduce over-level androgen, increasing
The number of globulin binding free testosterone (ovarian and
adrenal). In connection with the suppression of secretion estrogen
Gonadotropin decreases the formation of androgen.
Combined estrogen–Progestic contraceptives are the best
effective when taking high doses. Using low doses
Progestin, Northesis and DR. Provides the therapeutic effect only
After 2–4 months of reception, with their cancellation there are relapses. Most
Common drugs are ethinyl estradiol, ciproteron,
which are prescribed both separately and together. Systemic
Corticosteroids are used for adrenal hyperandrogenation.
Treatment with estrogen and antiandrogens lasts from several months to several years.
Antibacterial therapy has an important meaning in therapy
acne. Excessive amount of sebum, presence P.Acne for which
The listed conditions are a favorable environment, contribute
Development of pronounced inflammation. P.ACNE highly sensitive to different
antibiotics, but not all antibiotics are able to penetrate into
follicular apparatus, hasting gland, which depends on
efficiency.
Systemic antibacterial therapy suggests
Application of doxycycline, clindamycin,–Trimoxazola, erythromycin,
Tetracycline. Doxycycline, Minocyclin,–Trimoxazole is better soluble
in fats; It is proved that they are most effective compared to other
Antibacterial agents. Optimal doses of tetracycline and
Erythromycin – 500–1000 mg per day, doxycycline – from 100 to 200 mg.
When achieving a positive clinical effect (from 4 to 6 weeks,
Sometimes up to 4 months) It is advisable to reduce the dose.
To achieve a rack, long-lasting replay is necessary
The use of antibiotics by intermittent courses for a long time
of time.
With the intolerance of antibiotics, use is allowed
NS–Trimoxazole (trimethopris 80 mg and sulfamethoxazole 400 mg) 2 times
per day or trimethopris 100–200 mg per day.
Systemic antibacterial therapy does not exclude outdoor
Applications of antibacterial ointments (benzoyl peroxide and erythromycin,
Clindamycin) that are prescribed to 2–4 months for long suppression
Proliferation P.Acne. With severe cystic, pumping processes
Antibiotics are used in combination with corticosteroids.
In patients with cystic forms of acne, leaving the scar
Changes, keloid skin changes, hyperpigmentation when oral
Antibacterial therapy is achieved only partial remission. For
avoiding complications and optimal selection of therapy necessary
Purpose Isotretinoin.