How to diagnose thrombocytopenia? And how the treatment of thrombocytopenia is carried out? You can learn more about this from our article.
Content
Diagnosis of thrombocytopenia
 Many give inspection results, allowing to identify the pathology of the internal organs and diagnose the underlying disease of the body. Determination of the size and consistency of the liver, lymph nodes, palmar erythema palms, vascular stars, an enlarged spleen can help in the diagnosis of the disease. Identification of the pathology of the joints, skin, skeletal anomalies, analysis of neurological status is also very important. Not superfluous and regular thermometry to eliminate bacterial or neoplastic pathology. However, it should be remembered that a slight increase in the spleen available for palpation may be an option for the norm - the spleen is palpable in 10% of healthy children and in 3% healthy adults. Be sure to along with radiography of the heart and light ultrasound kidneys and, especially, liver. We observed cases of thrombocytopenia in the hemangiome of the liver and local consumption coagulopathy.
Many give inspection results, allowing to identify the pathology of the internal organs and diagnose the underlying disease of the body. Determination of the size and consistency of the liver, lymph nodes, palmar erythema palms, vascular stars, an enlarged spleen can help in the diagnosis of the disease. Identification of the pathology of the joints, skin, skeletal anomalies, analysis of neurological status is also very important. Not superfluous and regular thermometry to eliminate bacterial or neoplastic pathology. However, it should be remembered that a slight increase in the spleen available for palpation may be an option for the norm - the spleen is palpable in 10% of healthy children and in 3% healthy adults. Be sure to along with radiography of the heart and light ultrasound kidneys and, especially, liver. We observed cases of thrombocytopenia in the hemangiome of the liver and local consumption coagulopathy.
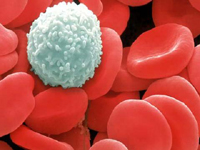
The main thing in recognition of the cause of thrombocytopenia still remains of laboratory research. The value of cytopenia, leukocytosis or abnormal leukocyte formula does not require a special conversation. Mandatory study of blade and creatinine blood is also not discussed. The need for sternal puncture by some authors is disputed. We believe that it is necessary in the first stages of diagnostic search, since some options for leukemia, pernicious anemia, debuting thrombocytopenia, as well as inherited forms of amgacariocytosis can be found only when analyzing Sterotinal Point. Research of platelet morphology necessarily (giant platelets and others.). Sometimes Tpanobiopia is required to confirm the bone marrow hypoplasia.
The determination of specific antibodies to platelet antigens, as well as the life expectancy of platelets, serum complement, direct anti-globulin test and the definition of IgG associated with platelets, is impractical to confirm the diagnosis of idiopathic thrombocytopenia.
Thus, the presence of thrombocytopenia obliges a doctor to make a conclusion about its character, determine its independence, and try to reveal the pathogenesis.
Treatment of thrombocytopenia
Treatment of hemorrhagic syndrome caused by thrombocytopenia always creates certain difficulties for doctors.
Before the start of treatment, it should be deleted primarily a secondary thrombocytopenia. Naturally, after establishing a diagnosis of secondary thrombocytopenia, treatment will be in the therapy of the underlying disease. However, with severe hemorrhagic syndrome, it is necessary to treat with a special focus on thrombocytopenia as the main cause of its. Let us dwell on the treatment of the most frequent ITP disease, detected by 96% of patients with thrombocytopenia.
The presence of thrombocytopenia in the patient often makes the physician of the first contact - a polyclinic, family or general practitioner - to take emergency measures not only in terms of examination, but also to prescribe medicinal therapy and almost necessarily hospitalize the patient. At the same time, long-term monitoring of patients with thrombocytopenia, especially with ITP, shows that emergency therapy is shown only with pronounced bleeding, which poses a threat to life. Patients without hemorrhagic manifestations with the number of platelets within 30 x 109 / l does not require hospitalization or treatment. Hospitalization is shown to persons with threatening life with bleeding, regardless of the level of thrombocytopenia, as well as patients with bleeding of mucous meters at platelet levels less than 20 x 109 / l and those who live far from the place of emergency medical care or differ in inadequate behavior.
Patient with a normal psyche and living there, where medical assistance can be provided immediately, hospitalization may be optional even if there are small hemorrhages at platelet levels of more than 20 x 109 / l. Serious hemorrhagic manifestations even at platelet levels within 10 x 109 / l occur only in 5% of cases, and at the level of 50 x 109 / l, even injuries are rarely complicated by pronounced bleeding. The platelet content below 10 x 109 / l is complicated by pronounced bleeding in 40% of patients. These considerations and determine the modern medical tactics of making patients with thrombocytopenia.
The proposed tactics can be briefly formulated as follows.
- If platelet levels exceed 50 x 109 / l, and hemorrhagic manifestations are absent or minimal, it is advisable to refrain from specific treatment.
- When the platelet level is below 20 x 109 / l, the patients show the specific therapy even in the absence of hemorrhagic manifestations.
- In cases where the platelet level of less than 50 x 109 / l, but there are additional risk factors of bleeding (arterial hypertension, stomach ulcers, as well as an excessively active lifestyle), treatment of thrombocytopenia should be carried out.
- If the level of platelets within 30 x 109 / l, there are no hemorrhagic manifestations, but the patient insists on treatment, it should also be carried out.
- Therapy should be prescribed in cases where the level of platelets is within (20-30) x 109 / l without clinical manifestations, but the possibility of emergency emergency care is absent in the patient.
- Platelet level (20-30) x 109 / l should also be an indication for patient therapy with inadequate behavior.
When the patient shows the treatment, medical science involves the following types of treatment: glucocorticoid therapy, intravenous administration of immunoglobulin, combined use of glucocorticoids and immunoglobulin, splenectomy, introduction of antuxus d-serum, flowing the thrombocytic mass.
Glucocorticoid therapy. Most patients respond to the treatment of glucocorticoids rapid lifting level of platelets. Dose of 1.5 mg / kg should not be considered more efficient compared to a dose of 0.5 mg / kg. The dose efficiency always manages to determine only empirically. The initial healing dose in an adult is 40-80 mg of prednisolone per day (15 mg every 6 h). Other glucocorticoids do not have any advantages compared to prednisolone. For intravenous administration, the hydrocortisone is preferred in a daily dose of 200 to 300 mg. This treatment must be carried out within 3-4 weeks. either before remission. The latter can be considered complete, if simultaneously with the cessation of bleeding, there is a rise in the number of platelets, or partial when the level of blood flow is not much changed significantly. After reaching remission, the daily dose of prednisolone can be reduced quickly - 5 mg per day to 30-40 mg. After that reduce the dose gradually - 2.5-5 mg of the drug per week. This type of treatment is almost always accompanied by undesirable phenomena: Kushingoid, arterial hypertension, diabetes, steroid ulcers in the stomach, increase body weight, cataract formation, osteoporosis, change of psyche. This can be observed after 20 weeks therapy prednisone even at a dose of 10mg / day. Unfortunately, after cancellation of treatment, the desired level of platelets remains less than 50% of patients. In practice, this effect of therapy has only 50 to 3% of treated patients.
 Intravenous administration of immunoglobulin may increase platelet levels in almost 75% of cases even with severe chronic thrombocytopenia.
Intravenous administration of immunoglobulin may increase platelet levels in almost 75% of cases even with severe chronic thrombocytopenia.
50% of patients marked the level of platelets almost to normal. Unfortunately, this treatment effect also turns out to be short-term. For the next 3-4 weeks. The platelet level is reduced almost to the initial in 75% of the treated. Up to 30% of patients treated with intravenous administration of immunoglobulin, in further steel resistant. The various mode of administration of the drug is described. Some authors offer to introduce it daily within 5 days at a dose of 0.4 g / kg. Others introduced a nearly similar dose - 1 g / kg for 2 days. One-time administration of immunoglobulin at a dose of 0.8 mg / kg gives the same results as previously presented treatment schemes.
Comparing the effectiveness of treatment with immunoglobulin and glucocorticoids, it can be noted that their action is almost the same.
Treatment with antibodies to the Rh Factor, Anti-Resh-D-Serum therapy. The experience gained to today's experience Anti-Resh-D Globulin allows us to say that it leads to the transient rise level of platelets by almost 50% of treated, this effect is held in the range of 2-3 weeks. This therapy is less efficient to the streets undergoing splenectomy.
Splenectomy in the treatment of thrombocytopenia is shown in the following cases:
- In the absence of an effect from the initially conducted drug therapy and the number of platelets less than 10 x 109 / l. In this case, the duration of the disease should be at least 6 weeks., And hemorrhagic manifestations may be absent;
- with the number of platelets less than 30 x 109 / l for 3 months. In the absence of their normalization, despite active therapy (glucocorticoids, intravenous administration of immunoglobulin, antibodies to the rhesus-d-factor). Splenectomy is possible both during bleeding and in its absence;
- In the absence of the effect of all other methods of treatment in persons with continued hemorrhage, which can be eliminated only by constant transfusion of platelet mass, while splenectomy is considered as a means «Latest hope»;
- Splenectomy is not shown as the first method of treatment.
In all other cases, thrombocytopenia splenectomy is not recommended.
Transfusion of platelet mass. It is believed that the transfusion of one unit of platelet suspension (5-10 x 1010 blood records from one dose of donor blood in 500 ml) should lead to an increase in platelet levels by 5-5-10 x 109 / l during the first hour. In the absence of this lift, the subsequent transfusions of the platelet mass are considered poorly oblated.
Other methods of treatment. Cases of effective treatment of thrombocytopenia with naiticoid, cyclophosphamide, vincristine, vinblastine, colchicine, a-interferon, cyclosporin, aminocaproic acid, plasmapherester, spleen irradiation, etc. However, to date, the effectiveness of none of these methods of treatment has not yet has serious confirmation in multicenter player-controlled studies.