Types of osteomyelitis: traumatic, hematogenic, chronic... Treatment of osteomyelitis.
Content
What is osteomyelitis
This is inflammation of bone tissue and bone marrow. Inflammation is usually developing due to the penetration of infection in bone tissue. Osteomyelitis, prevalence jaws occupies about a third of all osteomyelitis.
Depending on the source of infection, an odontogenic (source is a patient tooth), hematogenic (infection with blood flow from any organ) and traumatic (including firearms) osteomyelitis of jaws.
Types of osteomyelita
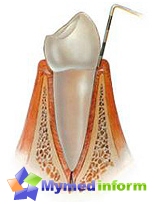
Odontogenous osteomyelitis of jaws - Pretty Terrible Complication of Launched Caries. This type of osteomyelitis occurs about 75% of cases of all osteomyelitis of jaws. Osteomyelitis develops due to the penetration of infection from the carious cavity, first in the pulp, and then through the root of the tooth into the bone tissue. About 70% of cases of osteomyelitis falls on the lower jaw and about 30% of cases of osteomyelitis - on the upper jaw. Etiology (reason) of odontogenic osteomyelitis - microorganisms of three groups: streptococci, staphylococci and some anaerobic bacteria. Microorganisms can penetrate bone tissue, both on bone canals and lymphatic vessels.
Hematogenous osteomyelitis Developed when infecting bone tissue by transferring infection from the primary focus of inflammation with blood flow. The source of infection is most often the foci of chronic inflammation, for example, chronic tonsillitis (chronic inflammation of almonds) and some other chronic foci of infection. Acute infections (scarletta, diphtheria, typhoid and even flu due to imminent impact) can also provoke osteomyelitis. Unlike odontogenic osteomyelitis, during the hematogenous version, the bone body is amazed first, after which it is possible to involve in the inflammatory process of teeth. The prevalence of hematogenic osteomyelitis is small.
Traumatic osteomyelitis develops during fractures and injuries due to driving infection in the wound. Its prevalence is also small and in sum with hematogenous osteomyelitis does not exceed 25% of cases. From the point of view of the clinical picture of the disease, the diseases are isolated, subacute and chronic osteomyelitis, which differ from each other severity (activity) of inflammatory processes.
 Acute osteomyelitis of jaws It is characterized by a pronounced reaction of the entire body for infection. Patients complain about general malaise, headache, weakness, bad sleep. The body temperature is increased to 38 s, but sometimes a higher temperature rise is possible. No temperature in the presence of other signs of the acute process indicates the weakening of the body's protective forces and requires a special approach to the treatment of patients. The condition of patients can be both light and heavy.
Acute osteomyelitis of jaws It is characterized by a pronounced reaction of the entire body for infection. Patients complain about general malaise, headache, weakness, bad sleep. The body temperature is increased to 38 s, but sometimes a higher temperature rise is possible. No temperature in the presence of other signs of the acute process indicates the weakening of the body's protective forces and requires a special approach to the treatment of patients. The condition of patients can be both light and heavy.
The first sign in acute odontogenic osteomyelitis is pain in the field of infected tooth. There is a sharp pain when tapping on the tooth, its moderate mobility is detected. Moreover, there is a mobility of neighboring teeth. The mucous membrane next to the tooth is edema, loose and red, painful when touched. Perhaps the development of substitute abscess, inflammatory contracts (reduction of mobility) of the lower jaw. In the palpation area of the neck, increased and painful lymph nodes mark.
The general view of the patient usually indicates signs of intoxication: adamina (lethargy), gray skin, pointed face rates, temperature rise). Possible jaundice eye sclera (if inxication affects the spleen and liver), protein and red blood cells in the urine (due to toxic kidney damage). Sometimes it is revealed to change blood pressure, both towards lifting and down. The picture of the blood is characteristic of inflammation: leukocytosis with a leukocyte formula shift to the left and elevated soe. On the first day of the acute reaction, the diagnosis of osteomyelitis of the jaw may be difficult due to the prevalence of common symptoms over local.
Subacute osteomyelitis Usually the next step in the development of acute osteomyelitis. Its development is associated with the facilitation of the patient's condition due to the breakthrough of the pus from bone tissue (usually in the oral cavity). There is a limitation of the melting section of bone tissue to form a characteristic picture of the sequestration. Inflammation does not disappear, but only «dulled», T.E. The destructive process in bone tissue continues.
Chronic osteomyelitis - The disease flowing for a long time, up to several months. At the same time, against the background of external recovery, there is an exacerbation of osteomyelitis, the formation of a new fistula, rejection of defective areas of bone tissue with the formation of sequesters. Self-esteem comes far from always.
Diagnosis of osteomyelitis of jaws Based on a clinical picture, data inspection, blood test, radiological picture of the disease and some other laboratory and clinical diagnostic methods.
Treatment of osteomyelitis
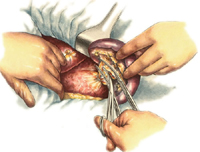
Treatment implies mandatory removal «Causal» Tooth (this is an example of an opportunity of absolute reading to the removal of the tooth). Early wide periodotomy (periosteum cuts) is shown to provide exudate outflow (inflammatory fluid). Antibiotics, disinfecting therapy, symptomatic therapy, as well as local therapy (bone cavity washing by antiseptics). Sometimes surgical intervention (deletion of sequesters), as well as bone plastic.