When I was pregnant for the first time, with this, I did not come across. But a few years ago, two prenatal screening were included in the framework of pregnancy - in I and II Trimesters. Order of the Ministry of Health of the Russian Federation from 2000 g. obliges women's advice to conduct biochemical prenatal screening to all pregnant women.
How to survive all related difficulties, I want to share our website with the readers.
What is Screening?

What is it? These are the so-called «double», «triple» and «Four» Tests that show those or other deviations of hormones during pregnancy.
Word «screening» translated as «screening», T.E. Of all pregnant women based on these indicators. The main purpose of screening is to identify groups of risk of developing congenital defects in the fetus - in particular, this is Down Syndrome, the vices of the nervous tube, Edwards syndrome. The result is calculated by ultrasound testimony and blood test taken from Vienna. Individual features should also be taken into account pregnant woman - its weight, age, smoking, therapy Hormonal drugs During pregnancy.
What we pass?

Like many other women, I was worried about the first screening - on ultrasound should see the so-called TVP (the thickness of the collar space), the indicator of which exceeding 2 cm (according to some data 2.5 cm) will indicate the possible presence of a dowan syndrome in a child. My child turned out to be well done, but as it turned out, it does not mean anything yet. By the way, I want to emphasize that the TVP must measure in a strictly limited period of pregnancy - from 11 to 14 weeks, but a genetic doctor in the center of immunology and reproduction told me that a more accurate result will be shot up to 12 weeks, the child will further grow up so much that in any case the size of the collar zone will not be informative. Blood in the first trimester for two hormones - B-HCH and PAPP-A.
For II screening (16-18 weeks) ultrasound procedure You can not do - readings for screening will take from the previous time. Blood surrender Already three hormones - B-hgch, afp and free estriol («Triple Test»), as an option, there is also the fourth indicator - Ingibin A.
Test results

So, analyzes and ultrasound are made, and now you are waiting for results. In women's consultation, they have to be expected for quite a long time - up to three weeks, if you pass screenings yourself, in paid laboratories, the result can be obtained pretty quickly - this is a question for one or two days.
And finally, the leafleka with the results you have. It shows the numbers against each indicator. But in order to correctly compare the indicators, they are not expressed not in absolute figures, but in IOM (multiplicity of median). Mediana is the average indicator for this marker on the specified period of pregnancy. The norm is MΩ ranging from 0.5 to 2.0. Deviation from these numbers indicates the possibility of pathologies.
Yes, this is what happened to me and happened. My indicators did not fit in the norm. Having shifted the sources (it turned out that they, unfortunately, not so much), I found out that the fallout could mean practically anything.
Increased hCG can talk about chromosomal defects, but also about multiplodies, and about rhesv conflict. But the reduction of hCG happens with ectopic pregnancy, the threat of miscarriage, not developing pregnancy. The increase and decrease in AFP will talk about fetal defects and possible chromosomal deviations.
And the presence of pathologies should be the combination of deviations in hormone indicators.
In the case of Down syndrome, for example, an AFP indicator is underestimated, and HCG is higher than the norm. Unclosed nervous tube, on the contrary, has a distinctive feature Elevated AFP and reduced hCG. But Edwards Syndrome is characterized by a decrease in the hormone studied.
And on the basis of these indicators on a paper with screening results, high letters is written - high or low risk. In brackets indicated the ratio, for example, 1: 100000 or, sadder, 1: 130 or 1:60. This means that 100,000 women with the same indicators will be born 1 child with this deficiency of development. The lower boundary is the ratio of 1: 250, t.E. Figure below 250 will indicate the high risk of presence of pathology.
If risk is high
When specifying a high risk, the doctor in women's consultation is obliged to send you to a consultation for a genetics doctor. Here you must make an important solution for you. Maybe the most important thing in life. Unfortunately, malformations for which risks indicate - non-treatable. You will only get the opportunity to know if you have «not like that» child.

Genetics will again look all the figures once again, asking you about your pedigree, whether you have taken hormonal treatment for pregnancy (in particular, many to preserve pregnancy take a urban or duphaston, which just cause an increase in the level of the HGG itself in the blood) But it will definitely tell you that there are no money to find out for the presence of pathologies in a child, except for invasive studies.
Screening only indicates the possibility of having a problem, but as we found out, deviations in the testimony can be caused incorrectly or not in time by the analysis or measurement of the TVP, or overweight at the mother, or by receiving preserving treatment. Detailed expert ultrasound examination aimed at a thorough study of the so-called pathologies, unfortunately, does not allow one hundred percent guarantee that there is or not a terrible disease in your child.
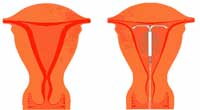
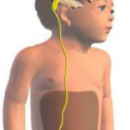
And in the event that the risk of your too high, the genetics will offer you an invasive study (invasion - penetration): biopsy of chorion, amniocentesis (fence of octoperwater water) or cordocentsis (fetal cord puncture). Depending on the type of research, they are conducted at different terms.
Here you can only solve you. Invasive studies - entirely and fully your decision, the doctor can only recommend them. Should you know for sure if it is necessary for you?
Yes, a certain risk in carrying out such procedures is. According to the doctors themselves, it is estimated depending on the method of from 2-3 to 0.5%. But if you decide on a similar study, our site recommends searching the place specializing in similar procedures - doctors there are extensive experience, qualifications, «Hand nailed».
A bonus in this study will be the exact news about - who is there who awaits you at the end of the way - a boy or a girl? When counting chromosomes, the error does not happen.
Summing up, I want to say with regret that screenings are still informative. If applied term «screening», then it is used with a solid with very large cells. The erroneousness of non-invasive studies is quite high. Not even all doctors have yet positively assess the mandatory. The topic is too scary, the future mothers are too worried and do not sleep at night, waiting for the results or trying to take the right decision. I myself cried at night for a month, trying to understand and interpret screening results and expecting counting chromosome... But my daughter is growing. No, now two daughters! And I hope and believe that over time, non-invasive screening will become informative and such research will help my daughters become happy moms.